By analyzing resting-state functional MRI (fMRI) brain scans with a machine-learning algorithm, researchers at the University of California, Los Angeles (UCLA) may have devised a way to predict treatment outcomes for people with obsessive-compulsive disorder (OCD), according to results published online February 12 in the Proceedings of the National Academy of Sciences.
By targeting functional connectivity between key brain regions, the algorithm identified two networks that were instrumental in forecasting which OCD patients would improve the most after therapy. If the findings are successfully replicated, they could lead to more efficient use of healthcare resources and faster recovery for people with OCD.
"We could potentially predict whether or not a person could be a responder to cognitive behavioral therapy and who may instead choose a different treatment option, perhaps neuromodulation or medication," said lead author Nicco Reggente, a doctoral student at UCLA. "Why go through the whole squeezing process if there is not going to be any juice?"
OCD fallout
Some 2% of people worldwide grapple with OCD over their lifetime. The disorder can lessen a person's quality of life, foster functional impairment, and destroy relationships. Cognitive behavior therapy is the most widely used form of treatment, but it is not always successful. It also can be quite time-consuming and costly.
 Nicco Reggente from UCLA.
Nicco Reggente from UCLA."In an ideal world, given an MRI is so expensive, a patient would come in who is looking to find some form of treatment for their OCD," Reggente said. "The best way this kind of paradigm could translate to a direct ecologically valid clinical application would be to see if we could predict how likely is the subject to respond to cognitive behavioral therapy or to medication."
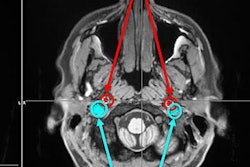
Enter the UCLA-developed machine-learning algorithm, which can be trained and tested repeatedly on a variety of subjects through "pattern learning," Reggente explained. By doing so, the algorithm can detect how well functional conductivity correlates to disparate regions of the brain throughout time in a resting-state fMRI scan.
"The degree to which [the algorithm] can learn depends on the patterns that you feed it, which is why we fed it different types of patterns from different cortical networks," he said.
For the study, the researchers recruited 42 subjects with a mean age of 32.4 years (± 9.9 years) whose OCD diagnosis was confirmed by one of the study's co-authors using the 10-question Yale-Brown Obsessive Compulsive Scale (Y-BOCS). The Y-BOCS test asks five questions about a person's obsessive thoughts and five questions about compulsive behaviors.
OCD severity is rated on the Y-BOCS from 0 to 40, with scores greater than 30 representing severe OCD. For this study, qualifying subjects had a score of at least 16, which indicates mild to moderate OCD.
The protocol for the fMRI scans included whole-brain 3D blood oxygenation level-dependent imaging (BOLD) for seven minutes on a 3-tesla scanner (Trio, Siemens Healthineers) with a 12-channel head coil (PNAS, February 12, 2018).
The 42 OCD participants underwent intensive cognitive behavioral therapy, which included 90-minute sessions five days per week for four weeks.
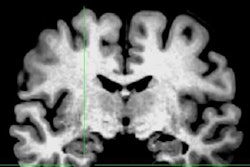
The algorithm evaluated patterns of functional connectivity in eight regions-of-interest (ROIs) in the brain during resting-state fMRI. The ROIs were selected based on a previous study that found significant pretreatment to post-treatment changes in connectivity in the frontoparietal, cingulo-opercular, somatosensory-motor, and visual networks.
"We did have a priori assumption, which is why we looked at different cortical networks that previously had been implicated in some form of aberrant activity that correlated well with OCD symptoms' severity," Reggente said. "We wanted to look at each of those networks and try to determine which has predictive power before treatment, [and] not just look at the scale of functional conductivity changes with their treatment."
The algorithm was trained on 32 subjects and then tested on the remaining 10 subjects, Reggente told AuntMinnie.com. The process was conducted "in an exhaustive way, so that every subject was in both the trained and tested groups. We ended up with a predictive score for everyone," he said.
Treatment predictions
In reviewing the Y-BOCS scores after treatment, the researchers found an improvement in 41 (97%) of the 42 subjects. Before treatment, patients had a mean Y-BOCS score of 24.6 (± 4.7), compared with a score of 15.0 (± 5.3) after treatment. The 39% reduction in mean scores of 9.8 (± 5.9) was statistically significant (p < 0.001).
As for the resting-state fMRI results, functional connectivity in the brain's default mode and visual networks was most predictive of a subject's treatment success.
With the addition of the machine-learning algorithm, connectivity in the default mode network successfully predicted 67% of the patients who responded favorably to therapy, while functional connectivity in the visual network accurately predicted treatment success in 51%. The other six ROIs had subpar predictive success; for example, activity in the frontoparietal network achieved only 21% accuracy.
"We were predicting that a least one of those networks, based on the previous literature, would have some predictive power," Reggente said. "The default network was predictive. That was not a real surprise, but the visual network was a bit more of a surprise."
More applications
Buoyed by the results of this proof-of-concept study, the UCLA researchers plan to conduct additional testing with more subjects. Their hope is that the application can be expanded to benefit those with other mental disorders.
"We would like to first replicate it and expand it on a new population of subjects, so we can feel confident that we are actually picking up on something reproducible and can be included in treatment programs," Reggente said. "Once this method is refined more and replicated and we get good feedback from it, then it is plug-and-play for other neurological disorders."
He cited patients with depression as one population that might benefit from an algorithm that can help predict response to therapy.
"If we look at functional connectivity within the default mode network and try to predict someone's responsiveness to treatment for depression, we can do that," Reggente said. "We just need data. What I am hoping for is that this method can be applied to a variety of medical disorders."