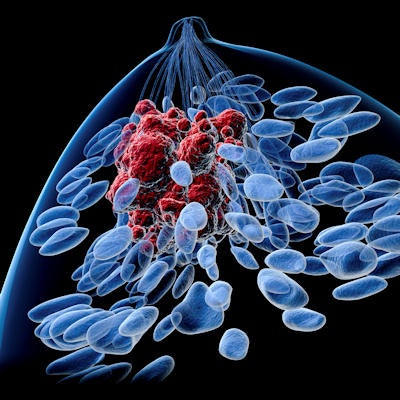
Follow-up imaging for women with nonmetastatic breast cancer varies widely across the U.S., with some women going without annual mammography postdiagnosis and others getting too much imaging via full-body scans, according to a study in the July issue of the Journal of the National Comprehensive Cancer Network.
Both the American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) recommend that women with nonmetastatic breast cancer undergo annual physical exams and mammograms but not full-body imaging with CT, MRI, PET, or bone scans. Yet more than a third of these women appear to be getting these higher-cost procedures anyway, wrote a team led by Dr. Benjamin Franc of the University of California, San Francisco (UCSF) (J Natl Compr Canc Netw, July 2018, Vol. 16:7, pp. 829-837).
Unnecessary full-body imaging exposes women to more radiation, and it's costly for those with high-deductible insurance policies, Franc said in a statement released by the university. Full-body imaging exams can cost between $2,000 and $8,000.
"With skyrocketing medical costs, patients have to take greater and greater responsibility for out-of-pocket expenses," he said. "And these patients already have cancer, so you don't want to induce another cancer with radiation from unnecessary imaging."
Franc and colleagues analyzed data from the Truven Health MarketScan Commercial Database, which includes information for particular metropolitan areas in the U.S. The study consisted of 36,045 women ages 18 to 64 who had surgery for cancer in one breast between 2010 and 2012; the team used an 18-month rather than a 12-month time frame to capture data for patients who had radiation therapy.
The researchers found that 71% of women received at least one follow-up breast exam after diagnosis, either a mammogram or a breast MRI. However, 32% had at least one high-cost imaging procedure and 12.5% had at least one PET scan -- neither of which is necessarily recommended, Franc and colleagues noted.
Younger patients and those who had radiation therapy were more likely to receive recommended breast imaging within 18 months of surgery, but the next most significant predictor was the patient's geographic area. The biggest predictor for PET imaging was the type of surgery a woman had undergone, followed by her geographic area.
Variation in follow-up also appeared as underimaging, with only about half of low-risk patients (that is, those who only had surgery) receiving recommended mammography within 18 months of their treatment. Percentages for high-risk women were somewhat better: 64% to 70% of those who had mastectomy and radiation received mammography or breast MRI 18 months after treatment.
The geographic factor was a surprise, Franc and colleagues noted.
"Age and therapy make sense as predictors of breast imaging, but it doesn't make sense that where you live makes a difference in whether you were likely to get a follow-up mammogram or high-cost imaging," Franc said. "[We] have these guidelines, but doctors aren't following them."