Using MRI instead of ultrasound to measure the wall thickness of carotid arteries can greatly improve the assessment of risk for adverse cardiovascular events and disease in people with no history of atherosclerosis, inflammation, or plaque formation, according to a study published online October 9 in Radiology.
In fact, MRI measurements with or without contrast were better than ultrasound measurements based on manual intima-media thickness for predicting coronary artery disease, stroke, and cardiovascular disease. The key difference is MRI's ability to image the thickness of the entire carotid vessel wall, which ultrasound cannot do.
"MRI is more consistently associated with cardiovascular events years later than intima-media thickness [with ultrasound]," said senior author Dr. Bruce Wasserman, a professor of radiology and radiology science at Johns Hopkins University. "However, the caveat is that we don't want to disregard conventional risk factors. So the question is: How much does MRI improve risk prediction by conventional estimators such as Framingham risk score? We should also consider that there have been advances in both MRI and ultrasound techniques since our study that may have improved risk prediction for each modality."
Within the wallsClinicians have relied primarily on ultrasound to measure carotid intima-media thickness when assessing a patient's level of early-stage carotid atherosclerosis. Among the modality's advantages are its low cost and noninvasiveness, as well as the absence of ionizing radiation and the lack of need for a contrast agent.
 Dr. Bruce Wasserman from Johns Hopkins.
Dr. Bruce Wasserman from Johns Hopkins.On the other hand, ultrasound measurements of carotid intima-media thickness are often limited to views of the artery's far wall. In addition, recent meta-analyses suggest that the modality's clinical efficacy "may be limited because it does not improve cardiovascular disease risk prediction beyond traditional risk factors in the general population," the authors noted.
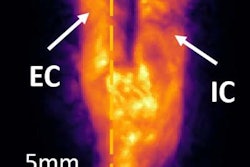
By comparison, MRI can image the circumference of the entire vessel wall, including the adventitia, or outer-most layer, which is not visible on ultrasound. The adventitia also is where small vessels proliferate, which could progress to thickening of the artery and result in vascular inflammation and disease.
"The focus of our research has been characterizing the vessel using high-resolution MR imaging," Wasserman told AuntMinnie.com. "That gives us insight into its thickness, which includes the adventitial layer, and the structure and components of plaque that might put it at risk for stroke."
MESA dataFor this prospective study, the researchers enrolled 698 men and women from the Multi-Ethnic Study of Atherosclerosis (MESA) between July 2000 and December 2013. Subjects ranged in age from 45 to 84 years (mean age, 63 years) at the time of their first imaging scans, and they had no known history of cardiovascular disease.
"One of the unique aspects of MESA is that it is a study of subclinical disease," Wasserman said. "These are asymptomatic individuals who have not had any overt manifestations of cardiovascular disease. This is a sample of our community that does not know they have atherosclerosis, so these are important people to study."
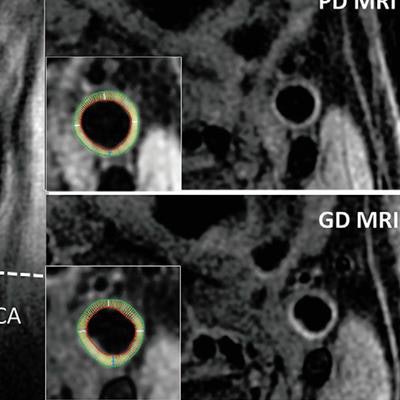
Participants initially underwent ultrasound and MRI exams between 2000 and 2004 to assess carotid artery wall thickness. MRI protocols included gadolinium-enhanced and noncontrast proton-density-weighted scans on 1.5-tesla systems with bilateral dedicated carotid coils at all six MESA sites.
The researchers then followed subjects with standardized MESA visits or by telephone every nine to 12 months. Most importantly, they recorded the onset of coronary artery disease, cardiovascular disease, and/or stroke, as well as death. The updates continued through the end of 2013 or until the subject died.
Risk assessmentsWasserman and colleagues found that noncontrast and gadolinium-enhanced MRI were much stronger than ultrasound intima-media thickness in linking vessel wall assessments with future adverse outcomes. Both noncontrast MRI and gadolinium-enhanced MRI performed particularly well in relation to stroke, compared with ultrasound.
| Ultrasound and MRI for predicting cardiovascular risk, by hazard ratio | |||
| Outcome | Ultrasound intima-media thickness | Noncontrast proton density-weighted MRI | Gadolinium-enhanced MRI |
| Coronary artery disease | 1.10 | 1.32 | 1.27 |
| Stroke | 1.08 | 1.48 | 1.58 |
| Cardiovascular disease | 1.14 | 1.37 | 1.38 |
"These findings suggest that wall thickness measurement by using MRI may be a more precise risk marker for coronary heart disease and stroke than intima-media thickness measurement by using ultrasound," the authors wrote.
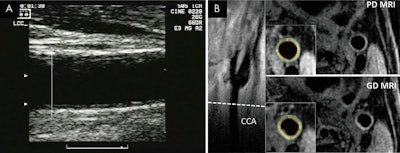 Ultrasound (A) and MR images (B) show common carotid artery (CAA) wall thickness assessment in a 62-year-old man. Intima-media thickness of the far wall was measured below the carotid bulb, starting where the outer wall of the artery begins to diverge (A). Corresponding MR images (B) show location of CCA section (dashed line) on long-axis view of left carotid bifurcation, with noncontrast proton density (PD)-weighted and intravenous gadolinium-enhanced (GD) MR images obtained at this location. Insets show inner and outer boundaries of segmented vessel walls, with white radial lines delineating 12 sectors over which wall thickness was computed. Images courtesy of Radiology.
Ultrasound (A) and MR images (B) show common carotid artery (CAA) wall thickness assessment in a 62-year-old man. Intima-media thickness of the far wall was measured below the carotid bulb, starting where the outer wall of the artery begins to diverge (A). Corresponding MR images (B) show location of CCA section (dashed line) on long-axis view of left carotid bifurcation, with noncontrast proton density (PD)-weighted and intravenous gadolinium-enhanced (GD) MR images obtained at this location. Insets show inner and outer boundaries of segmented vessel walls, with white radial lines delineating 12 sectors over which wall thickness was computed. Images courtesy of Radiology.As for the clinical implications of the findings, Wasserman advocated a "cautious and conservative" approach in how the carotid MRI technique is immediately applied.
"We don't want to overextend what we know and do not want to cross the line where we don't have evidence-based data to support [patient] management decisions," he said. "But I would say we might use it, for example, for certain instances where a patient comes in with more advanced carotid plaque that we think may be contributing to strokes, but does not qualify for surgery based on conventional angiographic criteria."
For more advanced plaques, which were not studied in this paper, Wasserman recommended a large surgical trial to validate the approach "before we can have a universally accepted protocol for managing disease using this technique."
"We do have pretty good data and we need to use it in some cases, but we are cautious in terms of how far we can go with it in making surgical decisions," he said.
The researchers cited several limitations of their study, including the relatively few cardiovascular disease events that occurred during follow-up. That dearth somewhat limited the researchers' ability to calculate subgroup analyses or to categorize wall thickness measures into quartiles to study the dose-response relationship.
"Because of the small number of events, our study may lack the statistical power to detect a significant association between intima-media thickness and cardiovascular disease outcomes," they concluded.