3D-printed models of human heads may remove the need for brain cancer patients to undergo a simulation CT exam before receiving whole-brain radiotherapy -- reducing costs and increasing workflow efficiency, according to an article published in the January issue of Technology in Cancer Research and Treatment.
Patients diagnosed with brain metastases on CT frequently elect to receive whole-brain radiotherapy as part of their treatment. Simulation CT scans are often acquired in addition to the initial diagnostic CT exam to assist with planning; clinicians use the simulation CT data to construct a personalized device for stabilizing the patient's head during radiotherapy sessions, noted senior author Dr. Philip Wong from the University of Montreal Health Center (CHUM) in Canada and colleagues.
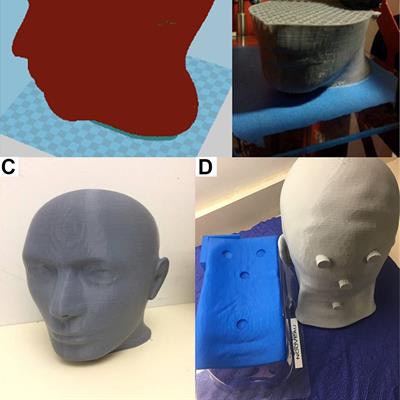
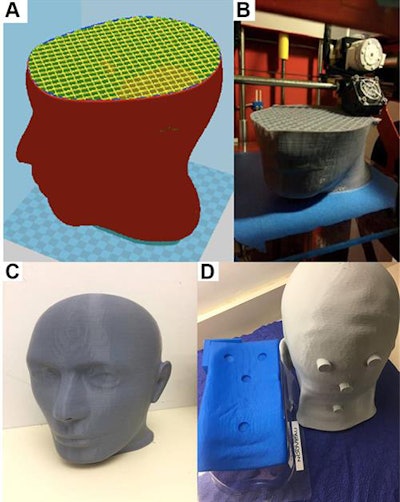 3D-printed head model and matching neck rest. Image courtesy of Wong et al. CC BY-NC 4.0.
3D-printed head model and matching neck rest. Image courtesy of Wong et al. CC BY-NC 4.0.Recognizing recent advancements in 3D printing technology, Wong and colleagues explored the possibility of using 3D-printed head models instead of data from simulation CT exams to design the immobilization devices.
To do so, they acquired the head CT scans of 11 patients scheduled to undergo whole-brain radiotherapy for brain metastases. They edited the scans using open-source software (3D Slicer) and a 3D modeling program (Catia, Dassault Systèmes), finally creating 3D-printed head models and matching neck rest models using a 3D printer (Technol Cancer Res Treat, January 2019, Vol. 17, pp. 1-8).
The researchers evaluated the accuracy of the 3D-printed heads by acquiring CT scans of the models and then co-registering the scans with the patients' simulation CT data. They found that each 3D-printed head demonstrated high similarity with the CT scans of the originating patient head.
On average, the 3D-printed models had a Dice similarity coefficient of 0.981 and an accuracy of 98.4%. The angles of deviation of the 3D-printed models from the original heads were also well within the 3° limit required for effective whole-brain radiotherapy. In addition, the mean percentage dose difference for radiotherapy between the dose measured on the 3D-printed head and the dose calculated on simulation CT scans was only -0.06%.
These figures suggest that the 3D-printed models resembled the head surface geometry of patients accurately enough for use in molding patient-specific thermoplastic immobilization masks for whole-brain radiotherapy, the authors wrote. Using this technique could remove the need for simulation CT and increase the availability of imaging for other patients.
The manufacturing cost for a 3D-printed head and matching neck rest was approximately $23, which was relatively cheap compared with the cost of a conventional simulation CT scan at their institution ($152-$305). At the same time, creating a 3D-printed head and neck rest takes roughly 36 hours, and so it would not be appropriate for patients requiring treatment within a shorter time frame, Wong and colleagues noted.
"The reproduction of a patient's head volume and position using 3D printing is feasible. ... This strategy could reduce the need for simulation [CT exams], thereby streamlining and simplifying the care pathways for patients with brain metastases," they wrote.



















