CT scans revealed rapid progression of abnormalities in COVID-19 patients, typically peaking on the 10th day from symptom onset, in a new study published March 19 in Radiology. The persistence of CT abnormalities through the final stages of disease underscores the need to monitor patients well after discharge.
Researchers from China examined the clinical and imaging data of 90 patients with COVID-19 pneumonia who were hospitalized and underwent multiple CT exams over the course of several weeks. The patients had their diagnosis confirmed by at least one positive reverse transcription polymerase chain reaction (RT-PCR) test and a CT scan showing lung abnormalities.
For this patient cohort, the researchers found that the CT findings followed a specific pattern from symptom onset to patient discharge. Two separate groups of radiologists with varying years of experience read the CT scans, quantified the data, and reported the following:
- Days 0 to 5: CT abnormalities progressed rapidly upon symptom onset. The predominant CT finding was ground-glass opacity in 62% of patients, followed by consolidation. Together, these two abnormalities constituted about 85% of all findings during this period. The distribution of lung abnormalities was bilateral in 85% of patients and often subpleural.
- Days 6 to 11: The CT abnormalities and involvement scores peaked for most patients on day 10. Ground-glass opacity remained the most prevalent finding at 59%, with a marked increase in the proportion of the pure ground-glass opacity subtype.
- Days 12 to 17: The severity of the abnormalities mostly persisted throughout this period, without any substantial change in CT scores or number of lung zones involved. Starting from day 12, mixed pattern became the second most prominent finding -- appearing in 38% of patients -- with ground-glass opacity falling to 45%.
- Days 18 to 24: Approximately 94% of the patients' final CT scans continued to show evidence of mild to substantial lung abnormalities. A reticular pattern also appeared in about 3% of the patients.
The radiologists also used a CT scoring technique to calculate the median number of lung zones affected (five out of a total of six, or three per lung) and lung involvement, which hovered around 25%.
A mixed pattern (i.e., a combination of ground-glass opacity, consolidation, and reticular opacity with architectural distortion) emerged at this point of disease progression in about 17% of patients. One person continued to show no CT abnormalities by day 11.
In addition, the researchers found an upsurge in the presence of ground-glass opacity in this late stage (61% of patients). Yet most patients were still discharged on day 24 after two consecutive negative RT-PCR tests.
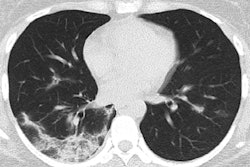
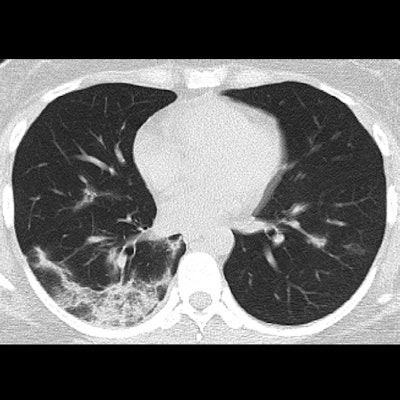
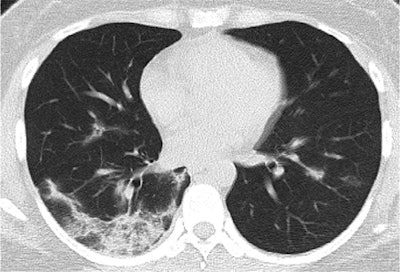 CT image from an exam performed on day 15 of illness in a 35-year-old woman with COVID-19. The image shows ground-glass opacity with a mixed pattern, and perilobular consolidation suggests possible organizing pneumonia. The patient was discharged two days later. Image courtesy of the RSNA.
CT image from an exam performed on day 15 of illness in a 35-year-old woman with COVID-19. The image shows ground-glass opacity with a mixed pattern, and perilobular consolidation suggests possible organizing pneumonia. The patient was discharged two days later. Image courtesy of the RSNA.Overall, the CT abnormalities and lung involvement progressed rapidly after symptom onset and peaked roughly six to 11 days later, followed by a persistence in high levels of lung abnormalities. The sensitivity of CT for COVID-19 was 84% during the first five days of illness and 99% from days six to 11.
"The temporal changes of the diverse CT manifestations followed a specific pattern, which might indicate the progression and recovery of the illness," wrote co-lead authors Yuhui Wang, PhD, and Dr. Chengjun Dong from Huazhong University of Science and Technology and colleagues.
Prior studies also have shown that some patients with COVID-19 can still test positive for SARS-CoV-2 as many as 13 days after being discharged with negative DNA results, they continued.
"Thus, follow-up monitoring of patients might still be necessary," the authors wrote.