Imaging and early antibiotic intervention saved the life of an 18-year-old man in Kansas who was diagnosed with Lemierre syndrome, or the "forgotten disease," after wisdom teeth extraction, according to a case report published on October 20 in the Cureus Journal of Medical Science.
The teen developed thrombosis of his superficial internal jugular vein after having his wisdom teeth removed. This is a rarely reported complication of this type of dental procedure, and few cases of Lemierre syndrome have occurred since antibiotics became readily available, the authors wrote.
"The presence of odontogenic infection with worsening pain and neck swelling should raise high suspicion to obtain necessary blood cultures and imaging for early diagnosis," wrote the group, led by Dr. Aarati Keshary of the University of Kansas School of Medicine.
Forgotten but there
Lemierre syndrome is a serious bloodstream infection commonly caused by Fusobacterium necrophorum, with a mortality rate of 18%. The syndrome was first reported in 1936, but a few years later, most antibiotic classes were discovered and introduced to the market, generally making it a disease of the past.
Oropharyngeal infections such as tonsillitis and mastoiditis most often trigger the syndrome, which leads to thrombophlebitis of the veins, specifically the internal jugular vein. The disease is uncommon and rarely arises from an odontogenic infection after teeth extraction, like in this case.
An 18-year-old man
When the teen presented to doctors, he had a three-day history of nausea and vomiting that started with pain and swelling in his left law. His medical history was unremarkable, but his wisdom teeth were removed 20 days prior.
His jaw was red and swollen. He had no fever, a rapid heartbeat, and low blood pressure of 98/57 mmHg. An exam revealed that he had diffuse lower abdominal and left upper quadrant pain.
His blood results showed leukocytosis of 30.0 x 103/µL with 35% bands, elevated creatinine of 2.64 mg/dL, and lactic acid of 2.3 mEq/L. His blood clotting profile showed an international normalized ratio of 1.5 and a partial thromboplastin time of 39.5 seconds, according to the authors.
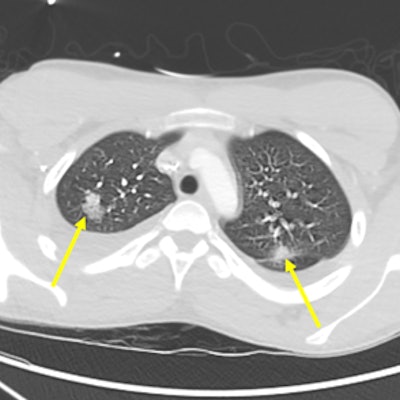
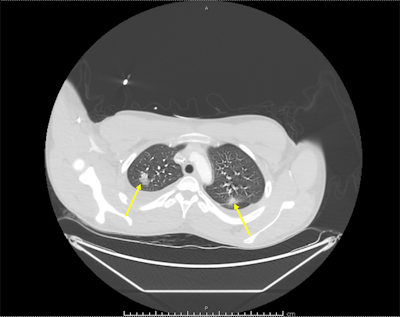 The arrows illustrate bilateral pulmonary infiltrates on a chest CT scan with contrast. Images courtesy of Keshary et al. Licensed under CC BY-NC 4.0.
The arrows illustrate bilateral pulmonary infiltrates on a chest CT scan with contrast. Images courtesy of Keshary et al. Licensed under CC BY-NC 4.0.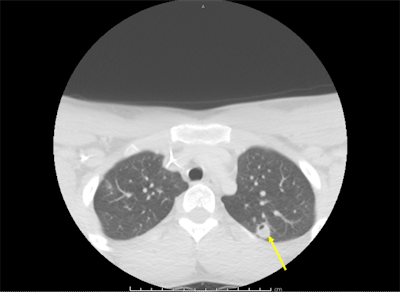 The arrow indicates interval development of cavitation that was later seen in nodular infiltrates consistent with septic emboli.
The arrow indicates interval development of cavitation that was later seen in nodular infiltrates consistent with septic emboli.Bilateral extraction of maxillary and mandibular molars and bilateral cervical lymphadenopathy were seen on a noncontrast maxillofacial CT scan. A noncontrast CT of his abdomen showed he had an enlarged spleen and a few tiny nodes in his mesentery. The teen was given intravenous antibiotics (vancomycin and piperacillin plus tazobactam) and fluid replacement, and he was admitted for further evaluation, according to the authors.
A setback
On his third day at the hospital, he was diagnosed with severe acute hypoxic respiratory failure and was intubated. He deteriorated rapidly, developing septic shock and multiorgan failure.
A neck ultrasound revealed a thrombosed superficial internal jugular vein consistent with thrombophlebitis, and a repeat chest x-ray showed right lung opacities indicating pneumonitis. A CT angiography (CTA) scan showed scattered nodular-appearing infiltrates throughout his lungs and moderate bilateral effusion. His blood tested positive for F. necrophorum.
Though the initial CTA failed to show pulmonary emboli, a subsequent CT scan showed evolving cavitation of the multiple nodular densities seen on the initial chest x-ray. The findings were consistent with septic pulmonary emboli. A vascular surgeon recommended that the teen's condition be managed without surgery.
The patient improved and was discharged after 12 days at the hospital. A CT scan was completed again at follow-up, which showed the jaw had a periosteal reaction. He was treated with six weeks of the antibiotic ertapenem. One month after discharge, imaging showed that the pulmonary infiltration and superficial internal jugular vein thrombosis had resolved, and the left mandibular osteomyelitis had improved.
Test quick, treat quick
The diagnosis of Lemierre syndrome depends greatly on clinical presentation with supporting blood culture and imaging results. Early intervention is key to treatment, according to the authors.
"Given the high mortality rate, emergent imaging is crucial, and there should be no delay in the initiation of antibiotic treatment," they wrote.



















