Using a streamlined breast MR protocol for women with dense tissue takes less time and finds more early cancers than mammography -- potentially replacing it as a screening modality, according to research presented at the RSNA 2012 meeting.
Another benefit? Rather than facilities spending more money on new technology, such as breast tomosynthesis, automated breast ultrasound, or contrast-enhanced spectral mammography, they could use existing breast MR units more efficiently, according to lead researcher Dr. David Strahle, president of Regional Medical Imaging in Flint, MI.
Strahle and colleagues found that using a limited number of MR sequences for women with 50% or more dense or fibroglandular tissue (by volume; i.e., how much dense tissue existed in the breast) identified an additional six cancers missed by mammography. This translates into 16.3 additional cancers per 1,000 women per year, according to Strahle.
"I'm convinced [the new protocol] will knock this disease out of the top 10 deadliest cancers category," Strahle told AuntMinnie.com.
Breast MR is currently used to evaluate the extent of cancer after it has been identified by screening mammography, according to Strahle. His study sought to identify cancers missed by screening mammography, to evaluate the role dense tissue plays in hiding breast cancer, and to determine if a new breast MR protocol could be developed for a national screening program.
"For almost 50 years, mammography has been the only screening imaging modality accepted on a national and worldwide level for early detection of breast cancer," Strahle said. "There have been little data available on the possibility of replacing screening mammography with breast MR -- until now."
Strahle and colleagues invited 671 women who had had a negative or benign screening mammogram between June 2009 and June 2011 to undergo a free breast MR. Women with recent positive mammograms, a personal history of breast cancer, who were BRCA-positive, or who had MR contraindications were not included in the study. For each woman, the researchers recorded data for 18 parameters, including percent volume and density of any fibroglandular tissue (FGT), location of any lesions inside or outside fibroglandular tissue, and the particular MR sequences of any lesions detected by the MR exam.
Detecting more lesions
Breast MR found 271 lesions not seen on screening mammograms in 250 of the 671 women. The lesions were characterized as follows:
- 80 benign solid masses
- 174 simple cysts at least 1 cm in size
- 2 ruptured implants
- 1 liver hemangioma
- 8 masses that did not meet benign criteria but were negative at biopsy
- 6 masses highly suspicious of malignancy
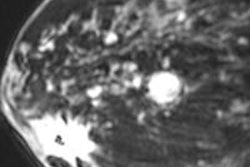
All of the six suspicious lesions were confirmed as cancers (one invasive lobular, three invasive ductal, and two ductal carcinoma in situ) in five women. All were hidden in fibroglandular tissue occupying at least 50% of breast volume regardless of the density of the tissue, according to Strahle.
"About half of our study population, or 369 women, had fibroglandular tissue equal to or greater than 50% by volume," he said.
Three MR sequences -- T1, T1 high-resolution, and T2 -- detected all of the cancers, and these sequences required only five steps, or only 12 minutes of scan time.
"Current breast MR sequences require 24 minutes of scanner time," Strahle said. "[The sequences we identified] significantly reduced the time and cost of a screening MR study."
Strahle's team did not consider any mass 5 mm or smaller as malignant unless the lesion showed unusual kinetic activity and a lobulated or spiculated shape and/or irregular or spiculated margins. The six cancers found by breast MRI were 7 mm, 8 mm, 15 mm, 41 mm, and 66 mm.
While this 5-mm threshold initially may not detect a few small cancers, it's reasonable to bypass these small densities for three reasons, Strahle said.
"The majority of them, if biopsied, would prove to be benign, significantly elevating the false-positive rate for very little gain," he said. "Small cancers not detected would eventually be detected by a change in size in subsequent years of MR screening. And the advantage of detecting cancers larger than 5 mm by MR outweighs the possible delay in identifying a few early cancers less than 5 mm, especially since screening mammography did not detect either in the first place."
In the study, breast MR had a false-positive rate of 57%, compared with 80% for mammography and 90% for mammography plus ultrasound. In the general population, mammograms detect 2.7 cancers per 1,000 women per year; from study data, Strahle extrapolated that the additional six cancers found by breast MRI would add up to 16.3 per 1,000 women with dense breast tissue per year (six cancers divided by 369 women with dense tissue greater than 50%, multiplied by 1,000).
"At the 2.7 screening mammogram cancer detection rate, it would take six years to identify all 16.3 cancers seen on breast MR," Strahle said. "Therefore, breast MR shifts time of detection six years earlier than screening mammography [in patients with dense tissue]. How many of the 40,000-plus women dying each year from breast cancer would shift out of the death category into the survival category if their cancers were picked up six years earlier?"
Small calcifications
Strahle did acknowledge that a potential drawback of using only MR for screening dense breasts is that some early cancers are identified by calcifications alone on mammograms; breast MR would miss these.
"These small calcified malignancies would eventually be detected by MR once they grew the required abnormal vasculature," Strahle said. "The advantage mammography has over MR in regard to these few small calcified lesions is clearly outweighed by the significant inability of mammograms to identify the majority of cancers obscured by dense fibroglandular tissue."
Screening mammography essentially seals the fate of women with dense tissue by delaying the time of discovery before MR can exert its influence to change the course of the disease, Strahle said.
"We're proposing a new, two-tier approach to early detection of breast cancer: Screening women who have greater than or equal to 50% FGT by volume with breast MR, then converting to screening with mammograms once tissue involutes below 50%," he said. "This two-tier approach can begin nationwide now, without having to purchase any new screening technology."