Although utilization of neuroimaging for ischemic stroke has increased sharply among Medicare patients, significant demographic disparities remain, according to research published April 25 in the Journal of the American College of Radiology.
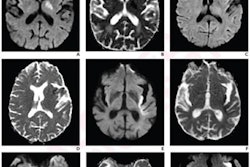
A team of researchers led by Jason Wang, PhD, of the Feinstein Institutes for Medical Research in Manhasset, NY, reviewed trends in stroke neuroimaging utilization and outcomes among Medicare patients from 2012 to 2019. They found significant increases in CT angiography (CTA), CT perfusion (CTP), and MRI over the study period.
However, neuroimaging was also performed less often on older, Black, female, and in particular, rural patients.
"Given these associations, understanding the root causes of the observed disparities is paramount to achieving equity in stroke care across the population," the authors wrote.
In an effort to update stroke neuroimaging trends, investigate socioeconomic disparities, and assess the impact of imaging on mortality, the researchers analyzed 85,547 consecutive ischemic stroke emergency episodes from the U.S. Centers for Medicare and Medicaid Services (CMS) 5% Research Identifiable Files.
They found significant changes in utilization for stroke neuroimaging from 2012 to 2019:
- CTP: +428%
- CTA: +250%
- MRI: +18%
- MR angiography (MRA): -33%
After performing logistic regression analysis and controlling for covariates, the team also found that the increased use of CTA and CTP were significantly associated with utilization of endovascular thrombectomy (EVT) and intravenous thrombolysis for acute treatment. This higher use had a positive impact on mortality.
In other results, the group determined that CTA, MRI, and MRA were all associated with lower mortality. However, CTP was associated with higher post-discharge mortality.
Wang and colleagues also found significant demographic disparities, most strikingly for rural patients, who experienced an increasing gap in use of CTA and CTP compared with urban patients over the course of the study period. Possible explanations for this disparity include rural hospital closures, disparities in time-sensitive access to imaging across facilities, lack of resources and underfunding, longer travel time for stroke patients to rural hospitals, and other factors that lead patients in rural communities to present outside the recommended stroke treatment time windows, according to the authors.
"The urban-rural disparity illustrated in our study has broader implications because previous studies have shown that low-income and marginalized populations are also more likely to seek care at low-volume hospitals," the authors wrote. "Many rural hospitals lack the angiographic equipment and personnel necessary to perform EVT procedures even if advanced CT imaging is performed."
Older (≥ 80 years), Black, and female patients also were significantly less likely to receive neuroimaging for ischemic stroke.
The study results also suggest that lower utilization of CT-based neuroimaging may translate to lower utilization of acute stroke treatment, according to the researchers.
"Whether these disparities impact acute stroke treatment utilization and clinical outcomes for disadvantaged groups warrants further study," the authors wrote.
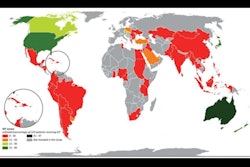
A significant disparity was also found when assessing neuroimaging utilization on a geographic basis. The highest CTA and CTP utilization was observed in the Northeastern and Western census regions, a finding that's likely related to regional variability in practice patterns and stroke care resource utilization, according to the researchers.
"This is highlighted by the fact that even with high relative CTA imaging, the Northeastern region still had the highest MRA utilization, which may imply duplicative testing," the authors wrote. "Consequences of this finding in terms of acute treatment utilization and outcomes should be investigated further."