Other Myocardial Imaging Agents
Tc-Teboroxime- No longer available for clinical use
Physiology & Pharmacology
Teboroxime is a neutral lipophilic boronic acid adduct of technetium dioxime (BATO) complex. Its uptake is proportional to regional myocardial blood flow and the agent has a high myocardial extraction fraction (about 90% which is higher than thallium). Additionally, extraction falls off less rapidly at high flow rates than sestamibi or thallium; thus this agent may be useful with pharmacologic stress agents as patients are not required to move between stress and imaging. The agent is no longer commercially available.
There is rapid myocardial washout- the myocardial T1/2 is 10 to 11 minutes (>70% washout) [1] and most of the administered activity is gone by 21 +/- 4 min. [2]. There is actually a biexponential clearance with a late T1/2 of about 80 minutes, but due to the initial major washout, insufficient activity remains for imaging. There is even quicker myocardial washout of the agent after stress imaging due to the increased blood flow.
The fast clearance may be because there is only a small amount of intracellular distribution when compared to Tc-Sestamibi or thallium, however, the compartments and mechanism of transport are not well established at this time. It is not known whether the agent enters the myocyte or remains attached to the phospholipid layers of the cell membrane. The small amount of agent remaining in the blood pool is altered into a form that does not undergo reuptake by the heart. Because of this rapid washout, high speed imaging devices are required. This does, however, offer the opportunity for rapid repeat studies. Washout of the radiotracer from the myocardium has been shown to correlate with blood flow. Clearance of the agent from ischemic regions is significantly slower when compared to normally perfused or infarcted myocardium. The faster washout from normal segments and slower washout from hypoperfused segments creates the appearance of defect reversibility on delayed images.
Excretion is enterohepatic, with peak hepatic uptake at about 6 min. following injection and there is more persistent retention of tracer activity within the liver in comparison to Sestamibi. The typical dose of Tc-Teboroxime is 30mCi (Dosimetry: Liver 1.9rad, Upper large bowel 3.7rad)
Technique
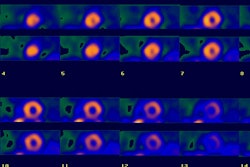
Separate rest and stress injections are required for imaging. Timing is crucial to obtain high quality images. Images must be obtained in the narrow time window between end of blood clearance and peak hepatic uptake. Acquisition should begin within 2 minutes of tracer injection and should be completed in less than 5 to 10 minutes after injection (this requires a 3 headed camera or a high count rate detector camera). Scatter from hepatic activity (esp. following the 2d injection) in the steep LAO oblique view can interfere with the interpretation of the inferoapical segments- esp. in obese patient's or those with high diaphragms. This can be minimized by acquiring the LAO view first, before liver activity peaks. Delayed scans will result in poor studies and defects can be missed. Generally, only planar imaging has been performed with this agent. This is because distortions are introduced during SPECT reconstruction when tracer activity is rapidly changing in the organ being imaged. Using a 3-headed camera complete acquisitions have been obtained in 2 minutes with no appreciable hepatic activity seen [3].
Sensitivity & Specificity
In a multicenter trial comparing Teboroxime and Angio/Thallium Zielonka, et al. found a sensitivity of 83%, and a specificity of 81% [4].
Tc-99m N-NOET
N-NOET is a neutral lipophilic myocardial perfusion agent which is being studied [47]. The tracer uptake is proportional to myocardial blood flow over a wider flow range compared to Tc-sestamibi or Tc-tetrofosmin [47]. The agent is bound to albumin in the blood and it appears to bind to endothelial cells (i.e.: it is not sequestered intracellularly) [47]. Myocardial clearance is increased by high circulating lipid levels and is also increased with prolonged hyperemia (as could be seen with dipyridamole stress) [47]. Similar to Tl-201 the agent will undergo redistribution, however, redistribution is much more rapid- with significant defect resolution by as early as 20 minutes following injection [47].
Fatty Acid Imaging
Free fatty acids (FFA) are the major source of energy for the myocardium in the fasting state [19]. Over 70% of the energy required by the normal myocardium under aerobic conditions derives from the metabolism of FFA [21,23]. A small amount of fatty acids are stored in the intracardiac troglyceride pool [23]. These stores serve as a buffer that compensates for short-term differences in FA supply and lipid oxidative demand and provide FA when plasma FA concentrations reach low levels [23]. Due to its small mass, the turnover of myocardial TG is quick [23]. Fatty acid oxidation generates about 6 times the ATP of glycogen oxidation [15]. Free fatty acids are transported in the blood bound to albumin [15]. Catecholamines increase the blood concentration of fatty acids [16].
Because free fatty acid metabolism is an obligatory aerobic process, it is very sensitive to reduced oxygen availability [20,27]. Myocardial uptake and retention of fatty acids has been shown to be affected by ischemia [15]. During ischemia, fatty acid metabolism is suppressed in a matter of seconds [16] and glycolysis becomes the predominant source of energy production for the sustenance of ischemic myocardium (glucose metabolism requires less oxygen consumption) [20,21,27]. The pattern of decreased fatty-acid use and enhanced glucose use is the metabolic signature of the ischemic heart [19]. Following an ischemic episode, abnormalities in fatty acid metabolism may persist long after perfusion has returned to normal (this is referred to as "ischemic memory" and can last several hours- even up to 24-30 hours in some cases [20,24,27])- during this time the myocardium garners the bulk of its energy from glucose metabolism [18,20].
I-123 IPPA (Iodophenylpentadecanoic acid)
I-123 IPPA is a single photon-labeled synthetic long chain fatty acid with kinetics similar to palmitate. Free fatty acids circulate in the plasma bound to albumin and cross the cell membrane by passive diffusion. Although the first pass extraction of I-123 IPPA is less than that for thallium, about 4 to 5% of the injected dose still localizes to the myocardium. Once inside the myocyte, the agent undergoes rapid clearance from the myocardium and this makes SPECT imaging a challenge [14,15]. I-123 IPPA is metabolized without iodine dissociation to iodobenzoic acid and its metabolite hippurate which are both rapidly excreted by the kidneys. Although there is only limited free iodine released, Lugol's solution should still be given prior to the exam to protect the thyroid [6].
Once inside the cell, fatty acids can either back-diffuse or become activated by acyl-CoA synthetase. Once the latter step occurs, fatty acids become polar and are trapped inside the cell where they can either undergo beta-oxidation (within the mitochondria) or be incorporated into the intracellular lipid pool. I-123 IPPA, like all fatty acids, undergoes biexponential clearance under normal resting aerobic conditions consistent with rapid early beta-oxidation (complete by 4 minutes) and a subsequent slower turnover of the remaining triglyceride pool.
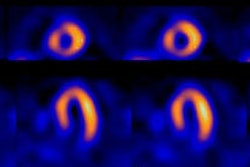
Myocardial ischemia inhibits fatty acid beta oxidation and will result in reduced uptake (due to diminished perfusion) and delayed clearance of tracer activity from these regions (prolonged myocardial retention is seen in ischemic regions on late imaging 120 minutes following tracer injection compared to non-ischemic regions) [10]). This pattern would also be observed in regions of hibernating myocardium. Infarcted myocardium demonstrates markedly reduced initial uptake of the agent, and no significant metabolism over time.
Using thallium reinjection imaging as the gold standard for viability, IPPA had a sensitivity of 90% and a specificity of 85%. IPPA detected viability in 23% more dysfunctional segments than reinjection thallium. Following revascularization, 80% of the IPPA viable segments demonstrated improved function, however, 33% of non-viable segments also demonstrated improved function [3,7].
Iodine-123-BMIPP (β-methyl-iodophenylpentadecanoic acid)
Iodine-123-BMIPP is a beta-methyl fatty acid analog in which methyl branching is introduced to inhibit β-oxidation (but this does not affect conversion to acyl coenzyme A) [9,11,12,15]. BMIPP undergoes slower oxidation and clearance by incorporation into the endogenous lipid pool which results in prolonged myocardial residence time (only about 25% of myocardial BMIPP is cleared in 2 hours [26]). Because the agent is retained in the myocardium for some time, it is more useful for SPECT imaging with a conventional gamma camera. BMIPP is usually injected under fasting conditions and imaging is performed 20-30 minutes after administration as earlier imaging reflects myocardial perfusion and may mask pure metabolic imaging [9,13,17]. BMIPP images are often compared with myocardial perfusion images in order to identify areas of perfusion-metabolism mismatch [26]. Approximately 0.2% to 1% of all patients who undergo BMIPP imaging demonstrate no accumulation of the agent in the myocardium [9]. This is likely the result of a congenital CD36 deficiency which is responsible for long chain fatty acid transport into the myocardium [13].
BMIPP is a very sensitive indicator of metabolic alterations in ischemic myocardium. In ischemic conditions (or in the state of heart failure) β-oxidation of fatty acids in the mitochondria is reduced with a shift to glucose utilization and subsequent back diffusion and early washout of non-metabolized BMIPP [12,13,26]. This decrease in fatty acid metabolism can persist for some time following the ischemic period- even after flow has been restored, and this is referred to as "ischemic memory" [26].
Areas with reduced uptake of BMIPP compared to the perfusion exam (ie: discordant BMIPP uptake) are felt to represent ischemic, but viable myocardium (such areas have been shown to demonstrate a metabolic-perfusion mismatch on PET studies) [8,9] and the finding is associated with regional wall motion recovery following revascularization [24]. Discordant BMIPP-perfusion uptake has been shown to be a strong predictor of future cardiac events [11,12]. Matching BIMPP-perfusion defects are indicative of scar and these regions are unlikely to recover function with revascularization [17]. Alternatively, patients with normal BMIPP exams have an excellent long term prognosis- cardiac event rate of 1% at 1 year and 4% at 5 years [12]. More BMIPP uptake than thallium perfusion is occasionally observed in the septal and inferior regions in healthy subjects, probably because of greater photon attenuation from thallium in these areas [9]. Comparison with Tc-99m-MIBI exams may help to minimize this effect [9]. Patients with CHF and decreased BMIPP uptake may be poor responders to beta-blocker therapy, whereas those with relatively preserved BMIPP uptake may respond well [17].
In a meta-analysis, for the detection of coronary artery disease
in patients with a high prevalence of CAD, BMIPP imaging had a
sensitivity of 78% (CI 73-81%) and a specificity of 84% (CI
77-89%) [19].
As BMIPP imaging can be performed without exercise or pharmacologic stress, the tracer may be of value for patients with acute chest pain (a metabolic defect will persist meven after symptoms have resolved) and those with contraindications to exercise and pharmacologic stress [19,27]. Studies have demonstrated an "ischemic memory" that can be imaged with BMIPP [22]. In the evaluation of patients presenting with unstable angina, rest BMIPP imaging can demonstrate metabolic defects in regions of normal perfusion consistent with an area of recent ischemia [22]. Adding BMIPP data to the initial clinical information increased the sensitivity for acute coronary syndrome from 43% to 83%, the NPV from 62% to 83% and the PPV from 41% to 58%, without a loss in specificity (61% vs 62%, respectively) [27]. Abnormal reduced uptake on rest BMIPP imaging in patients presenting with acute chest pain has been associated with a significantly increased risk for future hard cardiac events [24].
In hypertrophic cardiomyopathy:
In patients with HCM, abnormalities in BMIPP metabolism can be found in many LV segments with normal resting perfusion- particularly the most hypertrophied [25]. The abnormal BMIPP uptake is often most pronounced in the subendocardial regions [25]. The degree of regional LV BMIPP uptake has been shown to directly correlate with the peak negative myocardial velocity gradient measured by tissue Doppler [25]. Followup of asymptomatic HCM patients has shwon that abnormal BMIPP uptake at baseline can predict future deterioration in LV function [25].
REFERENCES:
(1) J Am Coll Cardiol 1990; Hendel RC, et al. Diagnostic value of
a new myocardial
perfusion agent, teboroxime (SO 30,217), utilizing a rapid planar
imaging protocol:
preliminary results. 16: 855-61
(2) J Nucl Med 1990; Stewart RE, et al. Myocardial clearance kinetics of technetium-99m-SQ30217: a marker of regional myocardial blood flow. 31: 1183-90
(3) J Nucl Med 1994. Murray GL, et al. Myocardial viability assessment with dynamic low-dose iodine-123-iodophenylpentadecanoic acid metabolic imaging: comparison with myocardial biopsy and reinjection SPECT thallium after myocardial infarction. 35 (Suppl): 43S-48S
(4) J Nucl Med 1995; Mahmood S, et al. Combined rest thallium-201/stress technetium-99m-tetrofosmin SPECT: feasibility and diagnostic accuracy of a 90-minute protocol. 36: 932-935
(5) J Nucl Med 1995; Cuocolo A, et al. Technetium-99m-tetrofosmin regional myocardial uptake at rest: relation to severity of coronary artery stenosis in previous myocardial infarction. 36: 907-13
(6) J Nucl Med 1995; Hansen CL, et al. Prediction of improvement in left ventricular function with iodine-123-IPPA after coronary revascularization. 36: 1987-1993
(7) J Nucl Med 1994; Hansen CL. Preliminary report of an ongoing phase I/II dose range, safety and efficacy study of iodine-123-phenylpentadecanoic acid for the identification of viable myocardium. 35 (Suppl.) 38S-42S
(8) J Nucl Med 1995; Tamaki N, et al. Decreased uptake of iodinated branched fatty acid analog indicates metabolic alterations in ischemic myocardium. 36: 1974-80
(9) J Nucl Med 2000; Tamaki N, et al. The role of fatty acids in cardiac imaging. 41: 1525-1534
(10) J Nucl Med 2002; Shi CQ, et al. Correlation of myocardial p-123-iodophenylpentadecanoic acid retention with 18F-FDG accumulation during experimental low-flow ischemia. 43: 421-431
(11) J Nucl Cardiol 2005; Tamaki N. Role of BMIPP imaging for risk stratification in patients with coronary artery disease. 12: 148-150
(12) J Nucl Cardiol 2005; Chikamori T, et al. Prognostic value of I-123 15-(p-iodophenyl)-3-(R,S) methylpentadecanoic acid myocardial imaging in patients with known or suspected coronary artery disease. 12: 172-178
(13) J Nucl Cardiol 2007; Chikamori T, et al. Diagnostic and prognostic value of BMIPP imaging. 14: 111-125
(14) J Nucl Cardiol 2007; Dilsizian V. Metabolic adaptation to myocardial ischemia: the role of fatty acid imaging. 14: S97-99
(15) J Nucl Cardiol 2007; Eckelman WC, Babich JW. Synthesis and validation of fatty acid analogs radiolabeled by nonisotopic substitution. 14: S100-109
(16) J Nucl Cardiol 2007; Bergmann SR. Imaging of myocardial fatty acid metabolism with PET. 14: S118-24
(17) J Nucl Cardiol 2007; Tamaki N, et al. The Japanese experience with metabolic imaging in the clinical setting. 14: S145-152
(18) J Nucl Med 2008; Vesely MR, Dilsizian V. Nuclear cardiac stress testing in the era of molecular medicine. 49: 399-413
(19) J Nucl Cardiol 2008; Inaba Y, et al. Diagnostic accuracy of β-methyl-p-[123]-iodophenylpentadecanoic acid (BMIPP) imaging: a meta-analysis. 15: 345-352
(20) J Nucl Cardiol 2008; Jain D, He ZX. Direct imaging of myocardial ischemia: a potential new paradigm in nuclear cardiovascular imaging. 15: 617-630
(21) J Nucl Cardiol 2008; Nishimura M, Ono T. Clinical utility of myocardial fatty acid imaging in patients with end-stage renal disease. 15: 830-837
(22) J Nucl Cardiol 2009; Beller GA. Can we enhance the detection of ischemia and better identify high risk coronary artery disease by imaging of myocardial metabolism? 16: 1-3
(23) J Nucl Cardiol 2009; Kisrieva-Ware Z, et al. Assessment of myocardial triglyceride oxidation with PET and 11C-palmitate. 16: 411-421
(24) J Nucl Cardiol 2010; Inaba Y, Bergmann SR. Prognostic value of myocardial metabolic imaging with BMIPP in the spectrum of coronary artery disease: a systemic review. 17: 61-70
(25) J Nucl Cardiol 2011; Shirani J, Dilsizian V. Nuclear cardiac imaging in hypertrophic cardiomyopathy. 18: 123-134
(26) J Nucl Cardiol 2011; Tamaki N, et al. Novel iodinated
tracers, MIBG and BMIPP for nuclear cardiology. 18: 135-143
(27) J Nucl Cardiol 2013; Gropler RJ. Recent advances in
metabolic imaging. 20: 1147-1172