The Thallium Rest-Redistribution Test
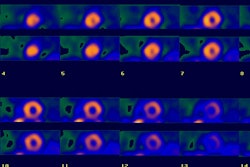
Rest-redistribution thallium imaging is used to assess for the presence of viable myocardial tissue with severely diminished perfusion (hibernating myocardium).
Technique
A rest-redistribution exam is useful when the clinical question pertains exclusively to the presence or absence of myocardial viability and not the detection of inducible ischemia. The exam is performed with a rest 3 mCi injection of thallium. Images should be acquired at the time of injection and 3 to 4 hours later. Reinjection prior to 4 hour delayed imaging is not performed and 24 hour delayed images are not required.
Findings
Three types of abnormalities can be identified:
1- Clearly reversible abnormalities
Indicative of severely ischemic, but viable myocardium (hibernating myocardium). Patients with areas of myocardial viability and left ventricular systolic dysfunction have been shown to have a much better prognosis when treated with surgical revascularization as opposed to medical therapy [3].
2- Fixed, severely decreased tracer activity
These areas most likely represent scar, although a small percentage (20%) show improved regional wall motion following revascularization [4]. When evaluating segments with fixed defects less than 50% of the maximal uptake, up to 25% have been shown to be viable by FDG imaging [5].
3- Fixed mild to moderate decreased tracer activity
About 50% of these regions show improved wall motion following revascularization which limits the predictive accuracy of the exam. These areas may contain mixed viable myocardial tissue and scar. Dilsizian feels that a Stress-Rest-Reinjection study may be beneficial in these patients. Ragosta feels that a mild defect (less than 30% reduction in activity) is indicative of viability.
Sensitivity & Specificity
The sensitivity of rest-redistribution thallium for the determination of viability and improvement in wall motion is 67%, and the specificity is 77% [11]. The rest-redistribution exam has positive and negative predictive accuracies of 69-72% and 70-92%, respectively, for the determination of recovery of regional left ventricular dysfunction following revascularization [1,2]. Although this is slightly less accurate than PET imaging (PET perfusion-metabolism imaging has a PPV and NPV of 76-83% and 84-92%, respectively [1, 2]), the cost and lack of availability of PET imaging limits its usefulness.
Rest-redistribution imaging does not necessarily provide the same information as a stress-rest-reinjection examination, although the two exams generally provide comparable information. One drawback of rest-redistribution imaging is that it may underestimate viability in 10% of defects in which thallium activity is severely reduced (less than 50% of normal activity). If there are no contraindications to stress testing a stress-rest-reinjection exam provides a more comprehensive assessment of the extent and severity of CAD by demonstrating regional myocardial ischemia, without compromising information on myocardial viability [6].
Quantitative analysis of rest-redistribution images may also be useful. A large percentage mild to moderate thallium defects (over 50-65% of maximal activity) on rest-redistribution images have been confirmed to be metabolically active on PET imaging. Sensitivity and specificity will vary depending on which threshold is selected [7]. Unfortunately, even in severe defects with less than 50% maximal uptake, metabolic activity has still been identified in up to half of these areas [8].
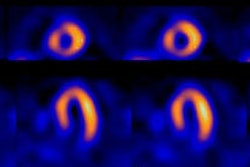
Reverse-Redistribution on Rest-Redistribution Exams:
(See also discussion of Reverse Redistribution in Stress Test section)
On rest-redistribution imaging two patterns of reverse-redistribution can be identified. In one pattern there is normal uptake on the rest image, but a defect is identified on the redistribution exam. This finding suggests a high grade stenosis in the vessel which supplies that segment. It is also frequently (up to 40% of cases) associated with impaired myocardial contractile function in the affected segment, but improvement in wall motion is very likely following revascularization.
In the other pattern there is a defect which is present on the rest image, but the defect demonstrates significantly decreased activity on the redistribution exam. Wall motion defects in these regions are more common (up to 60%), typically severe, and recovery of wall motion abnormalities following revascularization is very unlikely. Segments which demonstrate this finding should be classified as regions of scarring [9,10].
REFERENCES:
(1) Radiographics 1999; Jadvar H, et al. SPECT and PET in the evaluation of coronary artery disease. 19: 915-926
(2) J Nucl Med 1994; Maddahi J. Role of thallium-201 and PET imaging in evaluation of myocardial viability and management of patients with coronary artery disease and left ventricular dysfunction. 35: 707-15
(3) Chest 1999; Morse RW, et al. Rest-redistribution 201-Tl single-photon emission CT imaging for determination of myocardial viability. 115: 1621-1626
(4) Circulation 1993; Ragosta M, et al. Quantitative planar rest-redistribution 201Tl imaging in detection of myocardial viability and prediction of improvement in left ventricular function after coronary bypass surgery in patients with severely depressed left ventricular function. 87: 1630-41
(5) J Nucl Med 1995; Burt RW, et al. Direct comparison of fluorine-18-FDG SPECT, fluorine-18-FDG PET and rest thallium-201 SPECT for detection of myocardial viability. 36: 176-79
(6) Circulation 1993; Dilsizian V, Bonow RO. Current diagnostic techniques of assessing myocardial viability in patients with hibernating and stunned myocardium. 87: 1-20
(7) J Nucl Med 1998; Pace L, et al. Identification of viable myocardium in patients with chronic coronary artery disease using rest-redistribution thallium-201 tomography: Optimal image analysis. 39: 1869-1874
(8) J Nucl Med 1994; Hendel RC. Single-photon perfusion imaging for the assessment of myocardial viability. 35:(Suppl.): 23S-31S
(9) J Nucl Med 1993; Pace L, et al. Reverse redistribution in resting thallium-201 myocardial scintigraphy in patients with coronary artery disease: relation to coronary anatomy and ventricular function. 34: 1688-92
(10) J Nucl Med 1995; Pace L, et al. Reverse redistribution in resting thallium-201 myocardial scintigraphy in chronic coronary artery disease: an index of myocardial viability. 36: 1968-73
(11) J Nucl Med 1998; Bax JJ, et al. Comparison of fluorine-18-FDG with rest-redistribution thallium-201 SPECT to delineate viable myocardium and predict functional recovery after revascularization. 39: 1481-1486