SALT LAKE CITY - Twelve-month outcome data from the first patients treated with the Edmonton protocol for islet cell transplantation indicates that 8 of 10 patients with type 1 diabetes can achieve insulin independence with transplantation.
During a press conference Friday at the Society of Interventional Radiology (SIR) meeting, Dr. Richard Owen from the University of Alberta said 48 patients have completed the transplant procedure at Alberta Hospital in Edmonton, Alberta, Canada. "So far, 26 patients have reached the one-year mark and 21 of them are insulin free," Owen said.
Seven patients had transplants two years ago and four of them are insulin free, while four patients have reached the three-year mark and three of those patients remain insulin independent, he said.
Owen said that between 250 and 300 patients worldwide have already received islet cell transplants using the Edmonton technique.
Islet cells produce insulin, which allows the body to take sugar from the blood and supply it to cells, which in turn use sugar for fuel. At birth, a healthy pancreas has about 2 million islet cells, but when a person develops type 1 diabetes these cells are killed, which drastically reduces insulin levels and causes the sugar imbalance seen in diabetic patients.
Owen and his colleagues harvest islet cells from the pancreas in brain-dead donors. "You can see islet cells," he said. "They actually look like grains of sugar."
Patients require more than 4,000 islets per kilogram of their own weight. Typically, it takes "about 850,000 islet cells to achieve insulin independence," Owen said. Usually this takes more than one transplant.
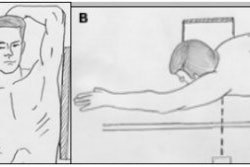
Using ultrasound or fluoroscopic guidance, the islet cells are delivered by catheter to the transhepatic portal vein. In the liver, the islet cells "immediately begin producing insulin," he said.
In the study presented at SIR, 90 transplants were performed in the 48 patients: 22 patients had two transplants, 10 had three transplants and 16 patients had a single transplant. "The transplant or infusion takes about 15 to 30 minutes," Owen said.
After the transplant all patients are placed on non-steroidal immunosuppressive therapy.
Currently, the only patients receiving transplants are those with labile diabetes, who can no longer be well controlled with insulin. These patients are at constant risk of losing consciousness because they can no longer detect when they have dangerously low blood sugar. "These people can pass out without warning, so they can’t drive, they cannot even walk around the block without putting themselves at risk," he said.
Owen said that transplantation appears to help these patients even if they cannot stay off insulin. "When they have to take insulin again, they are able to maintain good metabolic control, which suggests that the goal of this therapy might be either insulin independence or good metabolic control," he said.
In an interview with AuntMinnie.com, Dr. Michael Darcy, the current president of SIR, said that the Edmonton protocol represents a significant breakthrough in treatment of insulin-dependent diabetes, also known as type 1 diabetes or juvenile diabetes. But Darcy, who also is a professor of radiology at Washington University School of Medicine in St. Louis, cautioned that the treatment is still experimental. "We are, however, doing transplants at our institution and so far we have transplanted 12 patients," Darcy said.
By Peggy Peck
AuntMinnie.com contributing writer
March 31, 2003
Copyright © 2003 AuntMinnie.com