CHICAGO - Radiofrequency ablation isn’t just for livers anymore. The percutaneous technique is proving to be a viable option for zapping lung cancer, according to the results of a prospective multicenter trial led by Dr. Riccardo Lencioni from the University of Pisa in Italy, and joined by centers in Australia, the U.S., the U.K., and Austria.
In a presentation at Tuesday’s chest sessions of the 2003 RSNA meeting, Lencione said the CT guided interventional procedure yielded high tumor control rates with acceptable morbidity in patients with tumors 3.5 mm and smaller.
Lesions had to be at least 1 cm from major blood vessels or arteries, and the patients had to have sufficient blood platelets (> 100,000/mm3), and no prior pneumonectomy.
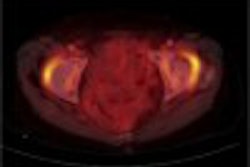
The ablation was performed using a 150-watt generator with 9 expandable multi-array needles or “hooks” (Rita Medical Systems, Mountain View, CA.) The system provided continuous monitoring of needle and tissue temperatures on a laptop computer, and the needles were configured to encompass the entire tumor, ablating an area 1 cm larger than the tumor itself, he said. The procedure was conducted under conscious sedation.
In all, 96 patients (ages 29-83) with 165 lesions (mean size 1.7 cm) underwent treatment. The tumors included 50 primary NSCLC in 31 patients; the rest were metastases, primarily from colorectal cancer. The largest tumor was 2.2 cm ± 0.7 cm; 13 of the 31 NSCLC patients had Stage I malignancies that were inoperable due to comorbidities, Lencione said.
To assess treatment response in the absence of a reliable imaging test, the group employed the RECIST response evaluation criteria for solid tumors. Designed for chemotherapy response, these criteria measure the shrinkage of tumors over time and therefore are not optimal for ablation. However, the RECIST criteria were still the best choice available, he said.
“So we assumed that lesions that did not show an increase of size or progressive disease during the follow-up had been completely ablated.”
Sixty-eight patients were followed up for 6 months, with results showing an ablation success rate of 89%, Lencione said. Results were similar for the one year follow-up. Follow-up ranged from 1 to 18 months; 44 patients underwent 1-year or more follow-up CT imaging, which showed a complete ablation rate of 90% in 53 lesions. Ten patients had locally progressing disease. (Follow-up CT of successful cases showed a ground-glass density area that progressively shrank.)
“When we compared the six-month follow-up to one year .. there were only two lesions that were seen to have complete ablation at six months and were in fact shown to have tumor regrowth (at one year),” Lencione said.
As for complications, they occurred in 15% of 121 procedures, including pneumothorax in 18 patients (the most prevalent complication by far) and pleural effusion in 6. Most of these resolved spontaneously, he said, and there were no fatalities.
“We think that based on these results, we can state that CT-guided RFA has high local tumor control rates, with a low complication rate and acceptable morbidity,” he concluded. “This technique may prove viable option eventually for NSCLC or other favorable histotypes or metastases, especially colorectal.”
By Eric Barnes
AuntMinnie.com
staff writer
December
2, 2003