As medical imaging goes increasingly high-tech, a new study out of the Netherlands indicates that the workhorse of radiology -- the chest x-ray -- remains a cost-effective exam that impacts patient management in a majority of cases.
In an article published in the August issue of the British Journal of General Practice, researchers from a multicenter group in the Netherlands sought to analyze the impact of chest radiography on patient management among a group of general practice physicians. The researchers were from the University Medical Centre Utrecht in Utrecht, Jeroen Bosch Hospital in 's-Hertogenbosch, Gelre Hospitals in Apeldoorn, and Onze Lieve Vrouwe Gasthuis in Amsterdam (British Journal of General Practice, August 2006, Vol. 56:529, pp. 574-578).
The researchers believe there has not been adequate study of the cost-effectiveness and clinical impact of chest x-ray in patients referred by general practice physicians, even though chest radiography accounts for 25% of all annual medical imaging procedures, and an average of 236 chest x-rays are performed per 1,000 patients per year in Western societies.
While some studies have analyzed the clinical utility of chest radiography, particularly in cases when abnormalities are detected, the authors sought to examine the impact of chest x-ray studies that have both positive and negative findings, and to analyze the effect that chest radiography had on patient management in general practice.
The study included 78 general practice physicians in the catchment area of one of the three main participating hospitals in the Netherlands, and was conducted from April 2003 to December 2004. The study included all patients age 18 years and older who were referred for chest x-ray to one of the participating hospitals by their general practice physician. The group started with a patient population of 870 patients; 78 were excluded from the study, leaving a final patient population of 792 patients.
The mean age of the patients at the time of their chest x-ray exams was 57.3 years, and 53% were male. Fifty percent had a history of cough, 25% of dyspnea, while physical examination found abnormalities in 40%. The most common suspected diagnosis was pneumonia (24%) and malignancy (18%).
The general practitioners were asked to fill out a standardized questionnaire before requesting a chest x-ray, including information on patient history and proposed patient management plans. The patient management section of the form was filled in as if no chest x-ray would be performed, with management options including referral to a medical specialist; initiation or change in therapy; reassurance of the patient; and follow-up by the general practitioner, including watchful waiting or additional diagnostic testing.
Patients were then referred for chest x-ray based on the general practitioner's referral. After receiving the radiology report, the physician was asked to fill out a second questionnaire that included the suspected diagnosis and anticipated patient management plan. Clinical findings were categorized into six groups: malignancy, pneumonia, chronic obstructive pulmonary disease (COPD)/asthma/chronic bronchitis, other clinically relevant abnormalities, the follow-up of abnormalities detected previously on chest x-ray, and no abnormality.
Patients received a short questionnaire six months after the chest x-ray to assess their perspective of the exam. Their possible responses included definite diagnosis, better treatment, reassurance, nothing, or other. The researchers used the questionnaire to measure the degree to which patients were reassured by the findings of the chest x-ray, and to compare it with the general practitioners' assessment of patient reassurance.
Of the 792 patients, 416 (53%) had no abnormality on their chest x-ray, while 179 (23%) were follow-ups of an abnormality detected previously on chest x-ray. Clinically relevant abnormalities were found in 197 patients (25%), including malignancy (n = 11, 1%), pneumonia (n = 44, 5%), COPD/asthma/chronic bronchitis (n = 99, 13%), and other clinically relevant abnormalities (n = 43, 5%).
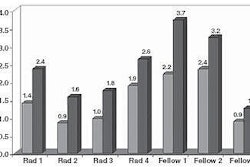
Chest x-ray resulted in a change in patient management in 60% of patients (95% CI = 57% to 64%). The main changes in patient management plans included a reduced number of anticipated referrals to a medical specialist, from 203 to 97; a reduced number of patients with initiation or a change in therapy (such as a reduction in the use of drugs like antibiotics) from 187 to 119; and more frequent reassurance of patients, from 195 to 363.
The authors said that while the study did not prove that patients benefit from chest x-ray in terms of traditional outcomes measures such as morbidity, mortality, or quality of life, it did demonstrate that chest x-ray often leads to changes in patient management, "which is one of the prerequisites for successfully influencing clinically relevant patient outcomes."
"Our results are in line with the conclusion ... that the clinical utility of (chest x-ray) was high enough to justify its costs," the authors stated. "This study showed that even after a history and physical examination of the patient the influence of (chest x-ray) on patient management was substantial."
By Brian Casey
AuntMinnie.com staff writer
August 11, 2006
Routine chest x-ray not needed after transbronchial biopsy, July 5, 2006
U.K. group finds high miss rate for lung cancers on chest x-rays, June 9, 2006
A checklist: Good for grocery shopping, but not for reading chest x-rays, March 13, 2006
WHO report: X-ray insufficient for TB diagnosis, March 29, 2006
Copyright © 2006 AuntMinnie.com