As 2012 draws to a close, AuntMinnie.com takes a look back at the year that was in our inaugural Year in Review special section. From concerns over procedure reimbursement to enthusiasm for the potential of mobile imaging, there was no shortage of big stories in radiology during the year.
No. 1: Reimbursement pressure weighs on radiology's recovery
The long-awaited recovery of the U.S. radiology industry never materialized in 2012, as continuing pressure on reimbursement created headwinds that were too strong to overcome.
Radiology has been mired in doldrums that began in 2006, when reimbursement cuts mandated by the U.S. Deficit Reduction Act (DRA) of 2005 went into effect. The specialty has had the misfortune of being cast as a bad guy in the drama over runaway healthcare spending, a debate driven by the fact that the U.S. lays out nearly 18% of its gross domestic product on medical care -- a level far higher than in other developed countries.
Indeed, what in radiology was considered to be the specialty's glory days -- the rapid growth in spending and utilization of the early 2000s -- was seen by policymakers as an aberration that needed to be hammered down.
And hammer they did. The reimbursement cuts of the DRA have been followed by a litany of additional payment cuts, rule changes, and technical adjustments that have slashed Medicare reimbursement while also trickling down to third-party payors.
 Radiology still bears the weight of reimbursement pressures.
Radiology still bears the weight of reimbursement pressures.
The result has been an industry that can't seem to get up off the mat. And the U.S. government doesn't seem to be letting up, with additional cuts proposed in the 2013 Medicare Physician Fee Schedule.
The irony is that by all accounts imaging utilization has dropped significantly from its peak in 2005. Several studies released in 2012 found that utilization of advanced diagnostic imaging has indeed plateaued, and industry groups such as the American College of Radiology (ACR) and the Medical Imaging and Technology Alliance (MITA) continue to press the idea that the reimbursement cuts are impeding access to imaging technology.
But are the feds listening? It's hard to say, but there are signs that federal legislators and policymakers may finally be gathering the willpower to at least consider changes to the in-office exemption to the Stark anti-self-referral law, which lets nonradiologist physicians purchase and use scanners within their practices with impunity. Recent studies have found that nonradiologist physicians have driven much of the growth in utilization as they grab market share from radiologists.
In 2013, look for movement in plugging the Stark loophole, as well as signs of "green shoots" that radiology could finally be in recovery mode. Radiology proponents are also developing better tools for managing utilization, such as the ACR Select program to put ACR Appropriateness Criteria at the fingertips of referring physicians via healthcare IT software.
By Brian Casey
No. 2: Radiation dose debate matures as new tools become available
The debate over radiation dose matured in 2012, moving beyond hysteria and into action. Gone were the headline-grabbing medical radiation accidents of previous years, replaced by determined action to bring dose down to the lowest possible level, and to use imaging more judiciously so patients aren't exposed to radiation unnecessarily.
Progress was made on multiple fronts during the year. In May, the U.S. Food and Drug Administration (FDA) launched a new program that will require scanner manufacturers to consider the safety of children when designing new devices, and California's landmark radiation dose reporting law went into effect in July. The Image Gently program brought its dose awareness message to new modalities during the year, and vendors continued to demonstrate impressive gains in dose reduction.
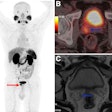
 Radiation dose continued to receive attention in 2012.
Radiation dose continued to receive attention in 2012.
Most of the debate in 2012 focused on CT dose. Radiologists with advanced CT scanners can now leverage a vast array of tools, many automated. These tools allow physicians not only to cut radiation dose, but also to reconstruct more readable images that increasingly highlight the most important data -- and in some cases let them compare their radiation dose data with that of other scans in other facilities.
Though new technical breakthroughs in 2012 seemed fewer in number than in the past, the year saw the beginnings of mainstream implementation of second-generation iterative reconstruction tools that had been rolled out in 2011 but remained mostly untested in daily clinical practice until now.
Thanks to programs such as Image Gently and other proponents of dose awareness, radiation exposure levels between and even within facilities are becoming standardized in efforts to eliminate outliers that can boost exposures unnecessarily. With the continued development of programs such as the ACR Dose Index Registry, imaging facilities are comparing their doses both internally and with other centers internationally.
This year also saw the emergence of more accurate radiation dose estimation, such as the size-specific dose estimate (SSDE), which uses patient size to adjust CT scanner protocols patient by patient. The development of dose reference values in the U.S., the increased use of tube current modulation and low-kV imaging, and research into spectral imaging techniques have all produced brilliant CT studies in specialized settings. Still, modern scanners offer so many dose-optimization tools that it's not always clear to radiologists which combination will produce the best result.
Impressive as these gains have been, however, they won't mean as much until they are implemented across the board; this year more than one study found evidence of wide variations in CT doses, especially outside of academic institutions. In 2013 and beyond, radiologists can hope for more guidance on maximizing the benefits of dose reduction tools, especially from the CT console. And they're likely to see more progress in protocol optimization and participation in dose registries.
By Eric Barnes
No. 3: Breast density movement snowballs as awareness grows
Since the state of Connecticut passed breast density notification legislation in 2009, the movement to inform women about their tissue density and potential increased risk for breast cancer has continued to gain momentum -- and doesn't show any signs of slowing.
There are currently five states with breast density notification mandates: California, Connecticut, New York, Texas, and Virginia. States that have endorsed notification bills include Kansas, Maine, Missouri, Nebraska, New Hampshire, Tennessee, and Utah, while Delaware, Michigan, Ohio, and Oregon have pending legislation. A federal bill was also introduced, but it's questionable as to whether it will make it through Congress during the current legislative session.
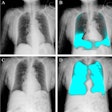
 Image with Volpara breast density score. Courtesy of Matakina International.
Image with Volpara breast density score. Courtesy of Matakina International.
As legislative work continues, medical organizations have begun speaking more frankly to the issue as well. In April, the American College of Radiology (ACR) released a breast density notification position paper stating that while the organization is not opposed to including breast parenchymal information in a patient's mammographic report, it's still unclear how patients may interpret breast density information and whether it is helpful. In November, the American Society of Breast Disease (ASBD) issued a document intended to help physicians notify women of their breast density status and explain how it affects their lifetime cancer risk.
The issue has begun to affect imaging vendors: GE Healthcare acknowledged that the snowballing breast density movement was a factor in its decision to acquire automated breast ultrasound (ABUS) developer U-Systems in November.
The issue of breast density was also prominent at the recent RSNA 2012 meeting. From the clinical perspective, many researchers shared data on the efficacy of additional screening tests such as ultrasound or breast MRI, and emphasized the need for standardization of breast density measures. In addition, from a social perspective, findings suggest that women with dense breast tissue are open to undergoing additional screening tests, despite the possibility of false positives, invasive procedures, and out-of-pocket costs.
In any case, there's no going back: Awareness of breast density, its risks, and the need for women to be informed if they have dense tissue is here to stay, according to Bonnie Rush, consultant and president of Breast Imaging Specialists of San Diego.
"While mammography remains a valuable and affordable early detection tool, breast density is now driving a crusade to develop and validate ancillary imaging tools to increase the viability of early-stage diagnosis," Rush told AuntMinnie.com."In this new paradigm, the successful breast imaging program will focus on a more personalized approach to breast imaging based on expanded risk profiling. The goal is personalized medicine and tailoring imaging protocols, rather than a one-size-fits-all approach."
By Kate Madden Yee