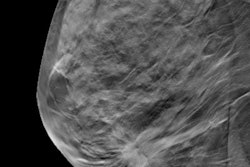
Women older than 75 received breast screening less often after they enrolled in an accountable care organization (ACO), found a study published online March 19 in JAMA Internal Medicine. The change was part of a general trend in which ACOs shifted cancer screening to conform with existing clinical guidelines.
In addition to declining participation in breast screening for older women, members of ACOs saw lower levels of prostate cancer screening, while colorectal cancer screening tended to shift toward those at highest risk of the disease, according to the study authors, led by Dr. Matthew Resnick of Vanderbilt University Medical Center (JAMA Internal Medicine, March 19, 2018).
But the new findings are drawing fire from breast imaging experts, who point out that recent studies have argued that if women are healthy and without other disease, breast cancer screening should continue past 75.
Accountable to whom?
The U.S. Centers for Medicare and Medicaid Services (CMS) developed the ACO model to promote improvements in the cost and quality of healthcare in exchange for shared savings between healthcare providers and payors. Early evidence suggests that enrollments in ACOs may reduce the use of "low-value" services, although little data exist that characterize the effect of ACO enrollment on the appropriateness of care -- that is, delivery of services to patients for whom the benefit exceeds the risk and withholding services from patients for whom the reverse is true, Resnick's group wrote.
"Effective cancer screening programs must balance the anticipated benefits associated with early cancer detection against the risks of diagnosis and treatment, with age and life-expectancy thresholds commonly used for screening recommendations," the team wrote.
The U.S. Preventive Services Task Force (USPSTF) currently recommends biennial breast cancer screening in women between the ages of 50 and 74; it states that there is insufficient evidence for screening in women older than 75. The task force recommends colorectal cancer screening in patients age 50 to 75 and is against routine prostate cancer screening.
Resnick and colleagues investigated whether Medicare ACO enrollment was associated with changes in the appropriateness of cancer screening using Medicare data from 2007 to 2014. The researchers measured annual rates of screening for these three cancers before and after the ACO structure was implemented and assessed whether any screening changes occurred in two age groups (65 to 74 years and older than 75); they also calculated predicted survival rates.
The researchers considered screening in beneficiaries between the ages of 65 and 74 to be appropriate and in those older than 75 inappropriate. The group found the following:
- ACO enrollment was not associated with higher breast cancer screening among appropriate candidates but was associated with a statistically significant reduction in screening among inappropriate ones.
- ACO enrollment was associated with improvements in colorectal cancer screening among appropriate candidates, with smaller magnitude increases in screening among those unlikely to benefit from early cancer detection.
- ACO enrollment was associated with a reduction in prostate cancer screening regardless of age or predicted survival.
| Effect of ACO enrollment on cancer screening rates | |||
| Cancer screening exam | Change in screening rates associated with ACO enrollment | ||
| Overall | Ages 65-74 | Over 75 | |
| Breast | -1.8% | -0.26% | -2.1% |
| Colorectal | -2.4%% | -0.36% | 0.08% |
| Prostate | -3.4% | -1.3% | -1.4% |
Cancer care is a key driver of Medicare spending, and, therefore, an important part of the ACO model, according to Resnick and colleagues. And there continues to be room for improvement for optimizing cancer screening.
"Of the $1.08 billion spent on breast cancer screening-related services, $410.6 million is spent on elderly women in whom there remains insufficient evidence to evaluate the benefits and harms of screening," the group wrote. "Medicare spends $450 million annually on prostate cancer screening, $145 million of which in men 75 years and older, unlikely to benefit from early detection. Indeed, a significant proportion of the U.S. population undergoes cancer screening regardless of mortality risk."
Disappointing findings?
But an editorial that accompanied the study lamented that the reduction in "inappropriate" screening wasn't significant enough. Allison Lipitz-Snyderman, PhD, of Memorial Sloan Kettering Cancer Center in New York City, described the findings as "disappointing," noting that the ACO enrollment effects Resnick and colleagues cited were modest at best. She also criticized the study's methodology, which consisted of comparing cancer screening differences before and after ACO implementation between ACO and non-ACO clinicians.
The breast screening community also might have choice words for the study. The underlying assumption by Resnick and colleagues that breast cancer screening in women older than 74 is "inappropriate" is simply wrong, according to Dr. Debra Monticciolo, chair of the American College of Radiology (ACR) Breast Imaging Commission.
"Breast cancer is the most common nonskin cancer in women and is a proven killer," she told AuntMinnie.com. "CISNET models, which are based on U.S. data, show that breast cancer screening is effective until age 80, and modeling teams have stated that benefits outweigh the risks up until age 90 -- so it is disappointing that [in this study] women over 74 are being discouraged from breast cancer screening."
In terms of breast cancer screening in particular, the study findings may say more about women who join ACOs than it does about the impact of ACOs on care, Monticciolo told AuntMinnie.com. And the assumption that older women are inappropriate breast cancer screening candidates -- one promulgated by the USPSTF -- does these women a disservice.
"The USPSTF continues to ignore the many observational trials that show benefit beyond age 74, the increasing life expectancy of our older Americans, and actual U.S. data that suggest benefits are significant for many older women," she said. "Older women should discuss the benefits and risks with their physician but should be encouraged toward screening if they are in good health and wish to remain so."