
Diverticular disease presents real challenges for virtual colonoscopy providers. Thickened haustral folds, fibrosis, pseudopolypoid lesions, and other structures can mimic colorectal polyps and tumors, resulting in false-positive findings and poor treatment decisions.
In the online edition of European Radiology, Dr. Philippe Lefere, Dr. Stefaan Gryspeerdt, and colleagues from Stedelijk Ziekenhuis in Belgium discussed a retrospective study of 160 patients with diverticular disease who underwent both virtual and conventional colonoscopy on the same day.
"Diverticular disease is the most common colonic disease in the western world, affecting 10%-30% of people at age 50, and 30%-60% at age 80," Lefere and colleagues wrote. Of this population 10%-30% will develop diverticulitis (European Radiology, e-publication before print, June 25, 2003).
The main predisposing factor is a lack of fiber in the diet, they stated. Other reported factors include increased consumption of red meat, fat, salt, and frequent use of anti-inflammatory drugs. Some hereditary disease such as Marfan's and Ehler-Danlos syndrome can also increase the frequency of the disease, as can immune suppression.
In the study, Lefere and colleagues reviewed 160 cases retrospectively (88 male and 72 female, ages 36-90). The patients had been referred for a history of polyps or colorectal cancer, family history, several abdominal pain, change in stool habits, or simply for being over 50 years old.
The patients were given a low-residue diet kit a day before the exam (Nutra-prep, E-Z-EM, Lake Success, NY), and underwent standard bowel prep with polyethylene glycol (Colopeg, Roche, Gaillard, France) bisacodyl (Dulcolax, Boehringer Ingelheim, Paris, France). Eight-five of the patients also ingested barium as a fecal tagging agent (Tagitol, E-Z-EM). Buscopan (Boeringer Ingelheim) was administered as an antispasmodic before the colon was insufflated to patient tolerance with room air.
The patients were scanned in the prone and supine positions on a single-slice scanner (Tomoscan AV/EU, Philips Medical Solutions, Andover, MA) using 5-mm collimation, 3-mm reconstruction interval, and 7/mm/sec table speed. The images were reviewed on a Philips EasyVision workstation.
The results showed diverticular disease in 89/160 patients (55.6%), including prediverticulosis (n=5, 3%) global wall thickening (n=89); diverticula (n=84, 52%), pseudopolypoid lesions including diverticular fecalith (n=63, 39%), One inverted diverticulum, and focal wall thickening (n=7, 4%).
 |
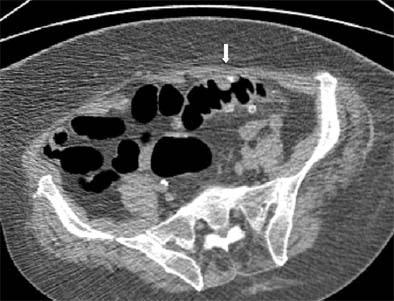
| Supine view: severe diverticulosis with global wall thickening and impacted diverticulum on the posterior aspect (white arrows). |
Prediverticulosis is the earliest stage of the disease, Lefere and colleagues wrote. It results from myochosis, a thickening of the muscular layer combined with foreshortening of the taenia and luminal narrowing that prevents the colon from elongating. When global wall thickening is seen, the myochosis has become more prominent, resulting in haustral abnormalities and reduced colonic distension.
"Although some authors have experienced improved colonic distension only by dual positioning and not by intravenous glucagon, we preferred to use smooth muscle relaxation to reduce patient discomfort and to avoid possible spasm..." they wrote.
 |
| Prone view: the sigmoid has flipped over its longitudinal axis, and better distension is obtained. A polypoid lesion remains visible (white arrow). Biopsy revealed only edematous mucosa and no polyp was detected. Images, courtesy of Dr. Philippe Lefere, were not included in the published study referenced herein. |
CT features of diverticular disease
Diverticula -- herniations of the mucosa, muscularis mucosae, and submucosa -- develop together with the myochosis, the authors explained.
"The diverticula are easily recognized as air-filled outpouchings of the colonic wall. On the (3-D virtual endoscopy) images, sometimes the orificium of the diverticular orificium can be recognized as a dark circumferential ring. Sometimes inflammatory changes with edema at the diverticular orificium can mimic a polypoid lesion," the authors said.
Pseudopolypoid lesions occur when diverticula become inspissated with fecal material, which can remain and harden into a fecalith, the authors wrote.
"Imaging findings are unequivocal when it presents as a hyperdense ring with a hypodense center on the axial images," the group wrote, adding that other researchers have reported different manifestations of impacted diverticula, such as barium or air attenuation, which did not render the findings equivocal.
However, soft-tissue attenuation can yield equivocal findings, and one group reported a thrombus filling the diverticulum after intra-diverticular bleeding as a possible pseudolesion, they stated.
Inverted diverticulum may also occur occasionally when the diverticulum is inverted into a pseudopolypoid lesion, the authors wrote. This can produce colonic bleeding, a result described by Dr. Seth Glick and colleagues as a 1.5 to 2-cm lesion with a central umbilication on double-contrast barium enema. (American Journal of Roentgenology, May 1991, Vol. 156:5, pp. 961-964).
"Imaging findings are unequivocal when on the axial images a sessile polypoid lesion contains some air due to a central umbilication in the inverted part of the diverticulum, or when it presents with a fat attenuation due to an inclusion of perisigmoidal fat," Lefere and colleagues wrote.
The 3-D endosocopic view shows an invariably polypoid shape, and therefore does not assist in diagnosis. In addition, inverted diverticula can be difficult to diagnose in the absence of air or fat.
"In conventional colonoscopy, inverted diverticula have been described to cause inadvertent diverticulectomy because of their pseudopolypoid appearance," the authors stated.
Polyp-simulating mucosal prolapse occurs when progressive diverticular disease foreshortens and contracts the muscular layer and taenia, causing an excess of mucosa to prolapse into the colonic lumen as a redundant fold, according to the authors.
This phenomenon creates pseudopolypoid or non-neoplastic lesions that usually have a broad base. Edema and recurrent bleeding can follow, and imaging findings are often equivocal.
"On axial and (3-D) images, they present as a polypoid lesion, (and) the polyp-simulating mucosal prolapse syndrome is indistinguishable from actual polyps," the authors said. Appearing as a hyperemic mass, such lesions are also difficult to distinguish in conventional colonoscopy, and sometimes only biopsy and histology provides an answer, they added.
Lefere and colleagues referred to one study suggesting that such lesions are quite common, appearing in 8/118 resected colon specimens (American Journal of Surgical Pathology, September 1991, Vol 15:9, pp. 871-878).
Focal wall thickening, caused by fibrosis, inflammation, or a tumoral process, presents on axial images as focal wall thickening without narrowing of the lumen, Lefere and colleagues wrote. And while a 3-D endoscopic view can help differentiate a thickened fold from a polyp, it cannot help differentiate fibrosis or inflammation from tumor.
"There is a significant overlap in the CT appearance of colonic carcinoma, inflammation, and fibrosis, with confusion in 50% of cases," they wrote, adding that diagnosis of tumor is 92% specific in cases when there is excessive wall thickening (>2 cm) with a short extension (especially with a shoulder formation or apple-core shape) and pericolonic lymph nodes.
Signs suggestive of fibrosis or inflammation are mild wall thickening (4-5 mm), a cone-shaped wall thickening, involvement of a long segment (> 10 cm), or fluid at the root of the mesentery. The diagnosis can be confirmed with conventional colonoscopy and biopsy.
As diverticular disease is common, it is important for providers to familiarize themselves with its imaging characteristics, the authors stated, noting that potentially equivocal imaging findings can be seen in any case of impacted diverticulum with soft-tissue attenuation, aspecific inverted diverticulum, polyp-simulating mucosal prolapse syndrome, or aspecific focal wall thickening. Equivocal and potentially significant findings should always be assessed with conventional colonoscopy.
"Although these findings will be rare in an asymptomatic screening population, radiologists should be concerned when confronted with these images...," they wrote. "Radiologists must be aware that examining a diverticular segment requires special attention because of the decreased visibility caused by a reduced luminal distension and muscular hypertrophy."
By Eric BarnesAuntMinnie.com staff writer
August 1, 2003
Related Reading
Virtual colonoscopy's tortuous path in diverticular disease, June 20, 2002
Copyright © 2003 AuntMinnie.com




















