MR virtual colonoscopy (MR colonography) continues to show promise as a tool for colorectal cancer screening, according to a presenter at the Royal Australian and New Zealand College of Radiologists (RANZCR) meeting last week in Brisbane, Australia.
Dr. Jörg Debatin from the University Hospital Essen in Germany said the two most important qualities of any screening test are diagnostic accuracy and patient acceptance -- requirements that MR colonography appears to fulfill. The procedure has been shown to be accurate for the detection of clinically relevant colonic polyps exceeding 10 mm in size, he said, with sensitivity and specificity values greater than 95%.
Debatin’s group performed MR colonography on patients after bowel cleansing. Patients were scanned in the prone position to enhance rectal filling, using a water enema (1000-2000 ml) to distend the bowel. Enhancement of the colonic wall was achieved through an IV injection of gadolinium-DTPA (0.2 mmol/kg).
The contrast agent had the effect of enhancing polyps more than the colonic wall, he said, adding that "3-D data acquisition was timed to coincide with the maximal contrast concentration in the interstitium of the colonic wall occurring at 75 seconds after completion of the IV contrast administration."
Fecal tagging obviates the need for colon cleansing before the MR examination, and also increases patient acceptance, Debatin said.
"For colonoscopy, the patients’ perception was that the worst part of the examination is the preparation, because they are medicated during the test," he explained. Because of the purgative cleansing, patients’ perceptions were that colonoscopy and virtual MR colonography were similarly inconvenient. So he believed that MR colonography without colonic cleansing might improve patient acceptance.
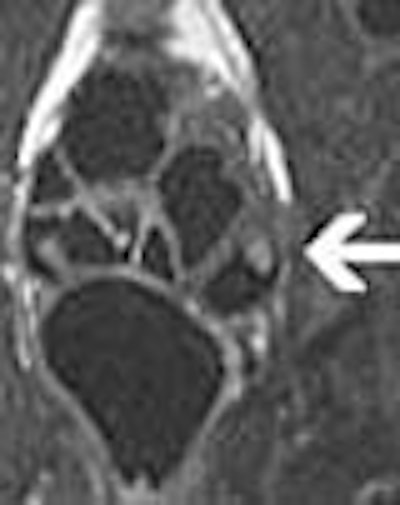
(Below, left) A single coronal 3-D GE MR image from a 71-year-old woman, acquired after administration of barium enema and IV gadobenate dimeglumine (Debatin 1). The arrow depicts a 2-cm mass arising from the enhancing colonic wall of the transverse colon, proximal to the splenic flexure. Histology confirmed the presence of carcinoma. Images courtesy of Dr. Jörg Debatin.
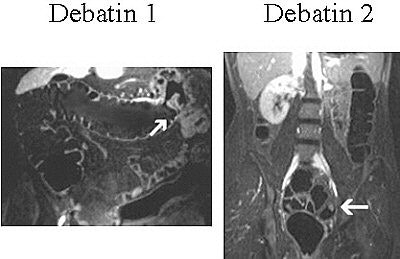 |
| (Above, right) A 33-year-old woman with a polyp in the sigmoid colon (Debatin 2). Single coronal MR image of a 3-D GE dataset, acquired after administration of barium enema and IV gadobenate dimeglumine, depicts enhancing 10-mm lesion arising from enhancing colonic wall in sigmoid colon (arrow). Images courtesy of Dr. Jörg Debatin. |
For fecal tagging, patients were given 200 ml of barium-containing contrast agent for four meals preceding the examination. "Beyond the elimination of foods with a high concentration of manganese such as chocolate or fruits, all subjects were free to choose their diets," Debatin said.
Because air, water, and fecal matter are all dark, bright polyps are well demonstrated against the dark background. Flat adenomas are small mucosal lesions that may not be recognized as polyps. They show a high degree of malignancy, but are difficult to diagnose because of a lack of protrusion into the colon.
"We are hopeful that the potential associated with this strategy will motivate others to join us in the quest to further develop and evaluate this technique," Debatin said.
Detailing further applications in the gut, he reported that true FISP (fast imaging with steady-state free precession) real-time MR imaging enabled the depth of gastric waves to be assessed. This provided functional information not previously available.
"Gastrointestinal dysfunction is the reason for 60% of visits to gastrointestinal (GI) doctors and 12% of GI-related hospital admissions," Debatin reported. Pathologies successfully evaluated by his department included dysphagia, dyspepsia, and irritable-bowel syndrome.
MR imaging of the small bowel normally requires intubating patients under fluoroscopic control in order to distend the small bowel, which can be difficult and uncomfortable. To address this issue, Debatin and colleagues investigated the use of various MRI oral contrast agents for inflammatory processes involving the small bowel, and established that the best distension was achieved using the following mixture.
Using a combination of locust bean gum (0.2%), mannitol (2.5%), a bulk fiber laxative, and water (1500 ml), his department successfully performed small-bowel MR imaging on 37 patients to assess Crohn's disease and lymphoma. Disease activity was assessed pre- and post-treatment.
MR imaging also can be used to assess obstructive processes such as pyloric stenosis and intussusception. To assess dynamic changes, patients were examined using a breathhold technique, antispasmolytic drugs, and water as a bowel contrast agent. MR sequences included the T2-weighted HASTE (half-Fourier acquisition single-shot turbo spin echo) and contrast-enhanced T1-weighted 3D-FLASH (fast low-angle shot).
By Leanne McKnoultyAuntMinnie.com contributing writer
October 2, 2003
Related Reading
German group optimizes barium-sulfate tagging in MR colonography, January 22, 2003
RARE technique shows benefits in MR colonography, July 15, 2003
Copyright © 2003 AuntMinnie.com