
Beyond screening for colorectal cancer and polyps, virtual colonoscopy could someday play a leading role in cancer staging. A new study from Italy suggests that, for at least the second time this fall, virtual colonoscopy has outperformed its conventional counterpart -- this time in patients with known or suspected colorectal carcinomas.
In a talk earlier this month at the 2003 RSNA meeting, Dr. Riccardo Iannaccone from the radiology department of the University of Rome La Sapienza discussed the results.
"Conventional colonoscopy and the double-contrast barium enema have several limitations, especially in that they cannot assess bowel-wall invasion or the presence of lymphoadenopathy and lymph (node) and metastatic disease," Iannaccone said. "As reported in the literature, CT and MRI also (have) limitations in the identification of both synchronous and primary ... carcinomas and/or polyps. So the purpose of our study was to assess the role of CT colonography in the detection and staging of colorectal carcinoma."
To that end, Iannaccone, Dr. Roberto Passariello, Dr. Andreas Laghi, and their colleagues in Rome recruited 150 patients who had lesions consistent with colorectal carcinoma at conventional colonoscopy. An additional 100 patients were included as a control group, Iannaccone said.
All patients underwent standard bowel preparation. The colon was insufflated manually with room air, and the antiperistaltic drug hyoscine butylbromide (Buscopan) was routinely administered intravenously prior to CT imaging on a Somatom Plus 4 Volume Zoom scanner (Siemens Medical Solutions, Erlangen, Germany). The protocol, used for patients with known or suspected colorectal carcinoma, calls for 4 x 1-mm beam collimation, a 1-mm reconstruction interval, 85-165 mAs, and 120 kVp.
"I would like to emphasize the use of a thin-section protocol, the use of (different) effective mAs in the prone (80 mAs) and supine (165 mAs) positions, and (the use) of intravenous contrast in the supine position only," Iannaccone said. Previous studies have shown that prone scanning produces superior distension of the sigmoid colon, he explained. At his institution, prone images are acquired first, then contrast is administered and supine scanning is performed after a 60-second delay.
Two experienced abdominal radiologists performed the image analysis on a dedicated workstation (Vitrea 2, Vital Images, Plymouth, MN) using a primarily 2-D approach. When a potential lesion was discovered, multiplanar reconstructions and endoscopic views were used for verification, he said.
"We evaluated the presence of lesions, as well as the stage of the neoplasm following the TNM staging system," he said. "CT colonographic results were subsequently compared with those of conventional colonoscopy and the results of the histopathic examination.... In particular, the reference standard for the evaluation of (VC) was a histological analysis performed on the suspected neoplasm. And lymph nodes were retrospectively analyzed. Metastases were confirmed though partial surgical resection."
The overall results showed 145 primary carcinomas, located in the rectum (n=13), sigmoid colon (n=58), descending colon (n=21), splenic flexure (n=9), transverse colon (n=10), hepatic flexure (n=5), ascending colon (n=12), and cecum (n=19). There were also five strictures due to chronic diverticulitis in the sigmoid colon, 14 synchronous carcinomas, 18 coexisting polyps confirmed and removed at conventional colonoscopy, and 32 liver metastases, Iannaccone said.
Of these, conventional colonoscopy found, "all primary carcinomas (145/145, sensitivity 100%)...however, we had inaccurate lesion location in five cases," he said. And due to the presence of obstructive neoplasms, "the procedure was incomplete to the cecum in 21 cases, and for this reason all (14) synchronous lesions were missed," he said.
Obstructing lesions weren't a problem in virtual colonoscopy, where "all primary and synchronous carcinomas (164/164) were correctly identified and precisely localized," Iannaccone said. "We also identified 21 polyps, although we had three false positives. So to summarize, we had a sensitivity of 100% for detection of carcinomas, and specificity of 97.2%."
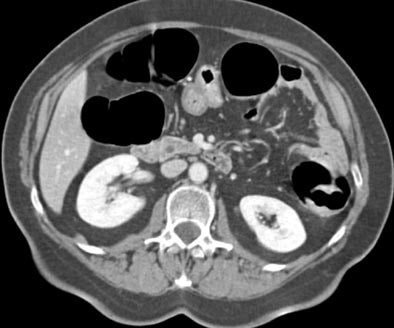 |
| Transverse MDCT colonographic image after contrast material injection. An occlusive carcinoma 3 cm in diameter is identified within the descending colon. The lesion was correctly staged as T2 at CT. Image courtesy of Dr. Riccardo Iannaccone. |
Commenting on one of the false-positive cases, he said, "We were convinced that this was an obstructive carcinoma, but histological analysis showed only inflammatory lesions and chronic diverticulitis in this patient."
As for staging, virtual colonoscopy correctly staged 131/145 primary tumors, for an overall TNM staging accuracy of 90.3%, Iannaccone said. T-staging accuracy was 87.8%, with three tumors overstaged and 15 understaged. Histopathology showed that one lesion thought to be stage 2 on VC was actually a stage 3 neoplastic microinvasion, he noted.
N staging was 94.4% accurate, and M staging reached 100% accuracy, "which means that (virtual colonoscopy) was able to identify both metastatic disease and metastatic lymph node involvement," Iannaccone said.
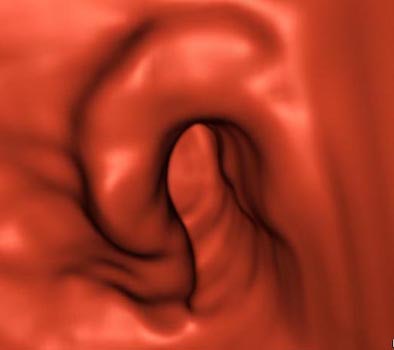 |
| Three-dimensional MDCT endoluminal view shows the morphology of the stenosing lesion with excellent detail. Image courtesy of Dr. Riccardo Iannaccone. |
"CT colonography correctly and precisely detected and localized all primary and synchronous lesions, providing correct staging in 90.3% of the cases," he concluded. "Therefore, considering the current limitations of other methods, CTC should be utilized as the first-line diagnostic test for patients with known or highly suspected colorectal carcinoma."
By Eric BarnesAuntMinnie.com staff writer
December 19, 2003
Related Reading
VC finds all masses after conventional colonoscopy fails in its mission, December 12, 2003
Virtual colonoscopy "almost ready" for widespread use as screening tool, December 12, 2003
Group credits 3-D reading for best-ever 3-D results, October 15, 2003
Virtual colonoscopy: to contrast, or not to contrast, April 10, 2002
Copyright © 2003 AuntMinnie.com




















