Without blowing things out of proportion, it's safe to say that insufflation is key to successful virtual colonoscopy. Adequate colonic distension is more important than thin-section imaging or even multidetector-row scanning, and ranks right up there with bowel prep in terms of the factors affecting lesion detection, according to Dr. Elizabeth McFarland.
McFarland, an associate professor of radiology at the Mallinckrodt Institute of Radiology and Washington University School of Medicine in St. Louis, made her point with a PowerPoint slide at the 2003 International Symposium on Virtual Colonoscopy in Boston.
"Small polyps can be seen even on two-row CT at 5-mm (slice thickness) with good insufflation, whereas in the areas of collapse we missed these lesions," she said.
More to the point, good insufflation doesn't just happen; it must be performed by someone who is dedicated and consistent, McFarland said. That person has traditionally been the radiologist, who can always learn a little more about the patient by doing the insufflation herself.
"But I think that with today's understaffing, we're learning more and more about how we can be more efficient," she said. "And from the success at the Mayo Clinic, and at (New York University), where they have dedicated CT techs to do this, we might start moving in that direction. Whoever does it, it's just essential to connect with the patient -- informing them of the duration (and) the importance of why they need it done. And try to reassure them up front (that) there's typically very minimal discomfort."
Positioning
In most patients, the initial filling begins with the patient in the right lateral position (right side down). This improves the flow of gas through the left-sided sigmoid-descending junction.
"If you think of it as a retrograde column of air that you're introducing, you (position) the sigmoid and descending colon (nondependently) in the left colon...which is smaller in diameter than the right colon...Usually give it about half of the full amount of gas you're going to give."
Then, after about 15-20 puffs, when the patients starts to feel the distension, move the patient into the supine position, according to McFarland. "That is not only the first scan position that you're going to do, but it moves that column of air to the non-dependent transverse colon," she said. "After you've introduced (gas) into the left side, then it goes to the transverse colon, then hopefully to the right colon. Then do the topogram."
With colorectal cancer screening volumes certain to continue growing in the future, virtual colonoscopy providers will eventually work their way down to patients who are harder and harder to insufflate and image. These patients may have already failed conventional colonoscopy, they may have already failed barium enema, and they may have few screening options left. As a result, taking the time to work with novel insufflation methods is a compassionate way to care for the patients who are most likely to benefit from virtual colonoscopy, McFarland said.
More difficult cases may need to be individually tailored. Some patients, such as quadriplegics and those who are very debilitated, often cannot be scanned prone, or may simply dislike the position. For these patients, initial insufflation in the supine position is often successful, followed by the change to left lateral decubitus position (left side down) to finish up. The advantage of this latter sequence is that it retains air in the transverse colon, McFarland said.
Generally speaking, after initial insufflation and imaging, the position for the second half of the exam should be tailored to the needs of the patient, she said.
Insufflation methods
Insufflation can be manual or automated, room air or CO2. One study by Dr. Judy Yee and colleagues showed improved distension with automated CO2 insufflation compared to manually insufflated room air. CO2 may also be more comfortable than room air because it is absorbed into the colonic mucosa. However, McFarland said a study by her group did not conclusively demonstrate a patient preference for CO2 (American Journal of Gastroenterology, March 2003, Vol. 98:3, pp. 578-85).
That study also noted that patients rated bowel preparation as the most negative part of both virtual and conventional colonoscopy. In considering future exams, patients favored CT (58%) over conventional colonoscopy (14%, with 28% expressing no preference), while overall appraisals of the just-completed exams were similar for both techniques.
"In the PLCO study, we showed a slight improvement of the overall subjective image quality in CO2 over air, very slight," McFarland said. "But there were no significant differences in the patient preference rating of air over CO2, and pain was none to mild for the majority of patients."
From the radiologist's viewpoint, "the manual puffs are certainly easy to administer," she said, while automated insufflation has the advantage of being able to deliver steady, continuous pressure levels. Because CO2 is absorbed, however, the radiologist must ensure that it is being delivered continuously, she said.
Experience has also led to higher maximum recommended pressures levels for automated insufflation -- from 14-15 mm/Hg a few years back to as high as 25 currently. At any rate, the lower maximum pressure settings often proved inadequate.
"We had some real failures in the tortuous colon or areas of fluid (with the lower setting), and if you reached that top pressure, the flow of CO2 was just cut off," she said.
For manual insufflation, about 40-60 puffs are typically required, she said, while an automated technique uses between 1.5 and 4 liters of CO2.
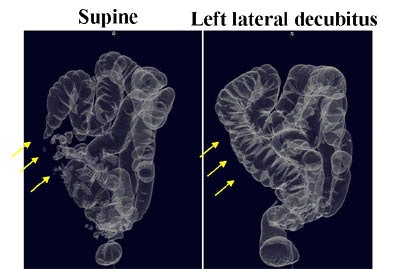 |
| Forty-year-old who had incomplete colonoscopy. At same-day virtual colonoscopy, the initial supine views (left) show incomplete distension of the right colon (arrows). At right, the use of left lateral decubitus (left side down) positioning achieved excellent right-colon distension. Images courtesy of Dr. Elizabeth McFarland. |
A study by Taylor and colleagues at St. Mark's Hospital in Middlesex, England, found that the use of inflatable balloon catheters did not significantly improve distension compared with the standard thin rectal tube. They also found the spasmolytic agent hyoscine butylbromide (Buscopan, Boehringer Ingelheim, Ingelheim, Germany) to be associated with improved colonic distension, while two concurrent studies found no improvement with use of the agent (Radiology, October 2003 Vol. 229:1, pp. 99-108).
"In the setting of diverticulosis, typically we do not use the (spasmolytic agent) glucagon," McFarland said. "But if it's a real diverticular hypertrophy, glucagon may help in selective cases."
When colonoscopy fails
In same-day virtual colonoscopy following a failed conventional exam, virtual colonoscopy is often performed 2-3 hours later. This can result in enormous variation in the amount of air remaining in the patient, and corresponding variability in how much additional insufflation is needed for VC, McFarland said.
"One woman, literally four hours later, was still so full of air that I immediately imaged her after the topogram, gave her no more (air), and the main thing I did for her was to give her that long rubber catheter to help decompress her (after the exam)," McFarland said.
Other patients might need 10-20 additional puffs of air before undergoing the virtual procedure, but again, the amount really needs to be tailored to the individual patient.
"So do a topogram early on," she said. "It's OK to start with a little bit of insufflation if they can tolerate it.... You've got to be careful you don't give them so much air that you see there's reflux into the small bowel, which makes the interpretation a little more tedious."
"In summary, insufflation is central for success," McFarland concluded. "We need to really tailor it to the patient, and today, remain open-minded in terms of the continual advances that are being made."
By Eric BarnesAuntMinnie.com staff writer
January 30, 2004
Related Reading
Jury deadlocks on use of Buscopan in virtual colonoscopy, September 18, 2003
Ultralow-dose virtual colonoscopy shows high sensitivity. April 8, 2003
Electronic CO2 insufflation beats air in virtual colonoscopy, March 12, 2003
Workflow issues key in virtual colonoscopy, January 15, 2003
Copyright © 2004 AuntMinnie.com