Immunocompromised patients are at high risk of invasive fungal infections, especially of the liver and spleen. Typical hosts include AIDS and marrow transplant patients, or patients with prolonged neutropenia. Candidiasis is by far the dominant filamentous fungal infection of the liver, but other forms, such as aspergillosis and zygomycosis in liver transplant patients, are appearing with increasing frequency.
Diagnosis has always been hit-or-miss. In fact, only about 9% of invasive fungal infections of the liver are diagnosed ante-mortem, according to Dr. Ur Metser, a radiology fellow at the University of Toronto. At the 2003 RSNA meeting, he presented a new study that relies on contrast-enhanced CT to diagnose infection and pave the way to antifungal therapy when appropriate.
"Fungal infection of the liver is one of the complications of prolonged neutropenia in patients treated for hematologic malignancies," Metser said. "Diagnosis is difficult because it's based on biopsy specimens, which are often negative.... Therefore, imaging plays an important role in both the diagnosis and follow-up of these patients."
The purpose of the study was to assess the clinical utility of bi- or triphasic CT (non-contrast, arterial phase and portal-venous phase) in patients with suspected fungal infections of the liver, based on the guidelines of the European Organization for the Research and Treatment of Cancer and Mycoses Study Group (EORTC/MSG).
The organization's guidelines came from a study in which "patients were proven positive for fungal infection, where 'proven' means aspiration of fungal cells from the liver, and 'probable infection' means unexplained fever during antibiotic treatment, abnormal liver function test, and proof of decrease in size or number of liver lesions on follow-up after antifungal therapy," he explained. The difficulty of obtaining positive biopsy results meant that only a few of the infections in the study were, in fact, "proven."
Metser and colleagues retrospectively examined 60 bi- or triphasic CT exams in the 39 immunocompromised patients with suspected fungal hepatic infections. CT images of the liver were acquired at 120 kVp, 230-330 mAs, table speed of 0.5 mm per rotation, high-quality mode, and pitch of 3:1. CT data were reconstructed using 5-mm-thick slices with 50% overlap. Nonionic intravenous contrast material was administered with the use of a power injector at a dose of 2 mL/kg up to a maximum of 200 mL, at a rate of 3 mL/sec with a 25-second delay for arterial phase, and 60-second delay for portal venous phase.
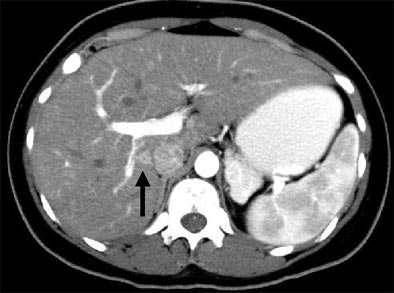 |
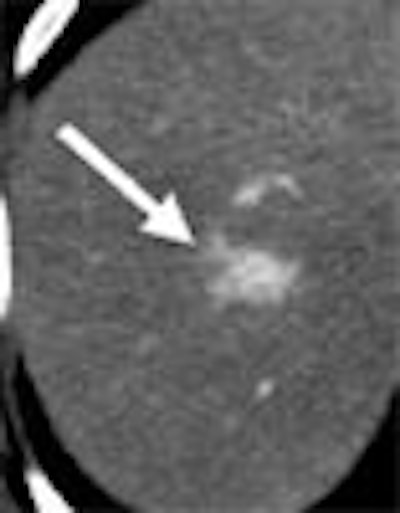
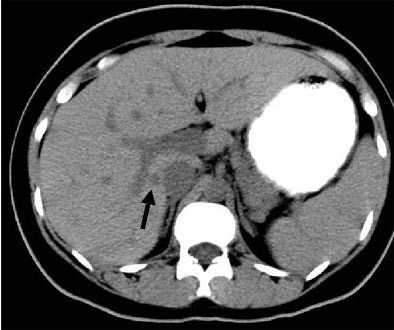
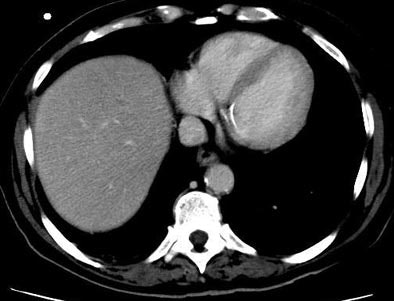
| Patient with fever after prolonged neutropenia. Above, arterial-phase CT of liver shows a type 2b lesion (arrow). Unenhanced CT (below) shows a corresponding hypoattenuating lesion, while portal-venous-phase CT (bottom) shows a tiny nonspecific hypodensity (type 1 lesion). This case demonstrates how arterial-phase CT adds specificity. Although portal-venous phase depicted the lesion, it would be extremely difficult to "call" it an abscess. The enhancement pattern on arterial phase CT makes for a more confident diagnosis. All images courtesy of Dr. Ur Metser. |
 |
 |
"All phases of all studies were randomized and presented to a panel of two radiologists who were blinded to the clinical and laboratory data," he said. "Decisions were made by consensus. The panel assessed the number of lesions in the liver, conspicuity on a four-point scale, (the presence of) focal splenic lesions, and the enhancement patterns of the lesion."
A phase was considered positive if at least three type 1 lesions, and one type 2 to 4 lesions, were identified. A study was considered positive if at least one of its phases was positive. And based on the available literature on fungal infections of the liver, type 2 and 4 lesions were classified as "lesions suggestive of infection," Metser said.
The four lesion types included:
- Type I: hypoatteunating (Ia= sub-centimeter in diameter; Ib= at least 1 cm in diameter);
- Type II: hypoatteunating center with a hyperatteunating rim (IIa= thickness of hyperatteunating rim equal to or less than the radius of hypoatteunating center; IIb = thickness of hyperatteunating rim is greater than radius of hypoatteunating center);
- Type III: any lesion with an associated transient hepatic enhancement (defined as an adjacent wedge-shaped region of increased enhancement);
- Type IV lesion: hyperatteunating lesion (brighter than surrounding liver).
The group performed a phase-based analysis of 536 liver lesions assessed in 36/60 positive studies. Arterial-phase CT identified all 36 (100%) of the positive livers, whereas the portal-venous-phase studies were positive in only 23/36 (69%) of the studies (p<0.001).
"On the lesion-based analysis, arterial-phase (CT) identified 90% (483) of 536 lesions assessed," Metser said, whereas portal-venous-phase CT identified 69% (329/536, p<0.001), and noncontrast CT 57% (265/465, p<0.001), he said. Focal liver lesions were graded as more conspicuous on arterial-phase and non-contrast CT compared to portal-venous phase.
"This example of a type 4 hyperdense lesion on arterial-phase (CT) is not seen on the portal-venous phase, and the follow-up arterial-phase (scan) performed a few weeks later shows that the type 4 lesion had changed its morphology to a type 2 lesion, with a central hypodensity and peripheral hyperdense rim," he said.
The study found that arterial-phase CT imaging detects significantly more hepatic lesions than other phases in these patients. The detection rates for arterial-phase and portal-venous-phase CT for the detection of focal lesions were not significantly different from each other, but both were significantly higher than noncontrast CT, he said.
 |
| Another patient with fever after prolonged neutropenia. Above, arterial-phase CT shows a type 2b lesion (arrow). Below, portal-venous phase fails to show a lesion. |
 |
The most marked difference between arterial and portal-venous phase CT could be seen in the detection rate for the hyperdense type 4 lesions, he said. On arterial-phase CT nearly 80% of the lesions had strong enhancement patterns suggestive of infection. Meanwhile, only 40% of the lesions on portal-venous phase CT had such a pattern, and only 45% of the type 4 lesions that could be seen on portal-venous phase CT had such a pattern.
"What's the rationale behind these findings? During neutropenia, fungal lesions may be invisible," Metser said. "Furthermore, documented lesions may become invisible if neutropenia recurs. Therefore the postinflammatory response plays an important part in defining the characteristic appearance of these lesions."
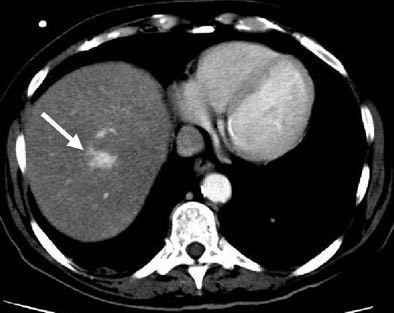 |
| Immunocompromised patient after prolonged neutropenia with fever and candidemia. Type 4 lesion on arterial phase (above) is not seen on portal-venous phase (below). The lesion was also not visualized in arterial-phase CT performed a few weeks earlier (bottom), indicating a new lesion. |
 |
 |
Arterial phase CT imaging increases sensitivity for the detection of focal liver lesions in immunocompromised patients with suspected hepatosplenic fungal infection, Metser concluded. "The addition of arterial-phase imaging could aid radiologists in making a more competent diagnosis."
By Eric BarnesAuntMinnie.com staff writer
February 17, 2004
Related Reading
Researchers determine optimal MDCT protocols for liver imaging, December 4, 2003
Saline flush boosts contrast enhancement in abdominal CT, November 6, 2004
For hypovascular liver tumors, late-phase CT is the way to go, August 18, 2003
Ultrasound effective in diagnosis, treatment of cystic liver lesions, May 15, 2004
Copyright © 2004 AuntMinnie.com




















