Unprepped MR colonography is a promising new tool for assessing inflammatory bowel disease (IBD) in children, according to radiologists at the University of Rome "La Sapienza" in Italy. The researchers considered that a noninvasive radiation-free exam that needed no prep might be just the ticket for improving the assessment of IBD in children, and perhaps its management as well.
"The role of MRI in the evaluation of small-bowel involvement in IBD has been well assessed in adults and also in the pediatric population, but what about the colon?" asked Dr. Pasquale Paolantonio in a presentation at the 2004 European Congress of Radiology in Vienna.
Indeed, MR colonography protocols are still taking shape, and can be performed in a number of different ways, he said. For example, MRC can differentiate the colon wall from stool and lumen on the basis of signal intensity, using either a bright-lumen or a dark-lumen technique. These components can also be differentiated by means of patient preparations. Some MRC techniques require bowel cleansing, while others do not, Paolantonio said.
"The aim of this study was to assess the feasibility of MRC performed without colonic cleansing by means of fecal tagging using oral administration of barium sulfate in a pediatric population with inflammatory bowel disease," he said.
The group examined 10 young patients between the ages of five and six years, all of whom had chronic diarrhea and proven IBD assessed at conventional colonoscopy with biopsies. The fecal tagging was performed by means of oral administration of 150 mg of highly concentrated barium sulfate at major meals, beginning three days before the MR exam. The patients also received, intravenously, 0.1 mmol per kilogram of body weight of gadolinium as a contrast agent. The colon was filled with a water enema immediately before MRI, which included the following sequences:
- T2-weighted HASTE (TR, inf; TE, 90 msec, FA 180º, acquisition time 20 sec.
- Contrast-enhanced T1-weighted 3D VIBE sequence (TR 5.2 msec, TE 90 msec, FA 180º, acquisition time 18 sec)
- T1-weighted 2D turboFLASH (TR 8.5 msec, TE 4 msec, FA 10º, 10 msec)
The images confirmed that the fecal material, bright without tagging, had been darkened by the oral barium to the point where it was indistinguishable from the water enema.
"There is optimal contrast resolution between the colonic lumen, that appears homogeneously dark, and the colonic wall," Paolantonio said. "The normal wall thickness was 100 mm. We looked for thickening of the colonic wall, we looked for (abnormalities) of the mucosal layer like pseudopolyps and like loss of haustral folds, and for parenchymal enhancement. Here you can see in this T2-weighted sequence some thickening of the colonic wall of the transverse colon with some pseudopolyps. These irregularities are shown also in this 3D reconstruction, with a good correlation to endoscopic view."
Image analysis showed that fecal tagging was optimal in all patients, and residual air did not cause any significant artifacts, Paolantonio said. Patient tolerance for the exam was high, and the final diagnosis was ulcerative colitis in seven patients and Crohn's disease in three patients. Unprepped MR colonography was able to define the thickening of the colonic wall and the extension of the inflammation following gadolinium injection.
"In the three patients with ulcerative colitis we observed a diffuse involvement of the entire colon from the sigmoid to the descending colon and the colonic wall was thickened and we observed stratification," he said. "In seven patients affected by Crohn's disease, the thickening was more focal."
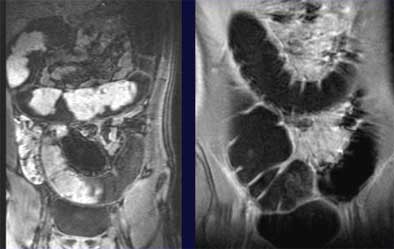 |
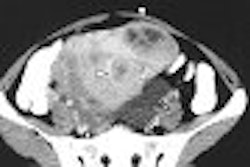
| Unprepped dark-lumen MR colonography technique shows normal subjects (colonic wall thickness < 3 mm) without (left) and with (right) fecal tagging. Fecal material visible in colon at left darkens to become indistinguishable from the water enema after fecal tagging, right, permitting assessment of the colon wall for IBD. Images courtesy of Dr. Pasquale Paolantonio. |
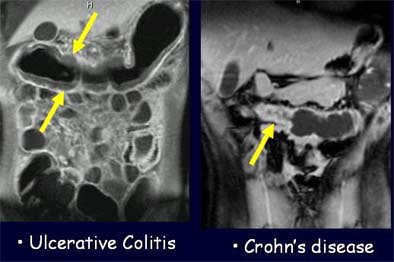 |
| Unprepped MRC technique shows wall-thickening patterns in patient with ulcerative colitis, left, and another patient with Crohn's disease, right. Images courtesy of Dr. Pasquale Paolantonio. |
Unprepped MRC using barium sulfate as a tagging agent is feasible and promising for the evaluation of colonic involvement in pediatric patients, Paolantonio said, particularly due to high patient compliance with the exam and its lack of ionizing radiation.
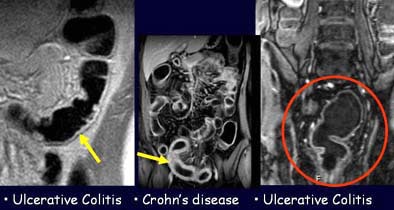 |
| The patient on the right is affected by ulcerative colitis, seen as a pattern of moderate colonic wall thickening and enhancement limited to the inner layer of the colon wall. The same pattern is present in the patient on the left side, who was diagnosed with ulcerative colitis involving the rectum. The patient in the middle is affected by Crohn's disease, and presents with more conspicuous thickening of the colonic wall and a transmural enhancement pattern. Images courtesy of Dr. Pasquale Paolantonio. |
"Further study is needed to evaluate the potential clinical role, especially in the recruitment of patients for conventional colonoscopy, the follow-up, and the therapies (needed) for successful treatment," he said.
By Eric BarnesAuntMinnie.com staff writer
July 12, 2004
Related Reading
New tagging, subtraction techniques aim for better compliance in VC, March 8, 2004
German group optimizes barium-sulfate tagging in MR colonography, January 22, 2003
Copyright © 2004 AuntMinnie.com