
Esophageal cancer, a disease that is highly curable when caught early but usually fatal when advanced, presents a thicket of diagnostic and treatment challenges. A wide array of treatment options, especially for early stage disease, makes accurate staging crucial for optimizing outcomes.
But imaging modalities have offered only partial solutions. The ultrasound gold standard is fairly dependable for detecting and staging small, localized tumors, for example, but cannot reliably evaluate advanced disease. CT is better for stage T2 and beyond, as it can depict the invasion of muscle wall and adjacent organs. But it often misses smaller lesions, and sometimes overstages T2 tumors as T3 when the muscle wall cannot be visualized. MRI's sensitivity has trailed that of CT in some studies, and can also have a tendency to overstage. Other studies show that PET, and especially PET/CT, have yielded better staging results than CT alone.
Now researchers from Japan are improving CT's ability to stage esophageal cancer, with new techniques and findings presented at the 2004 RSNA meeting in Chicago. First, researchers from Kyoto University Hospital in Kyoto, Japan, compared arterial- to venous-phase imaging for esophageal cancer, and found that arterial-phase imaging was far superior in spotting earlier disease. And a team from the Graduate School of Medicine at Chiba University in Chiba, Japan, used ECG gating to reduce motion artifacts in assessing pericardial invasion of advanced esophageal cancer, with impressive results in a small cohort of patients.
Arterial-phase imaging improves early stage detection
"Endoscopic ultrasound is usually adequate for the evaluation of local extension of the (esophageal) tumor," said Dr. Shigeaki Umeoka from Kyoto University and Kyoto University Hospital in his RSNA presentation. "Although CT has been used for parenchymal evaluation, it has limitations, (including) overstaging, especially in small tumors, due to its low contrast-to-noise ratio."
The development of multidetector-row CT has improved the modality's ability to image the entire esophagus, but it remains unresolved whether arterial- or venous-stage imaging in particular might improve accuracy, especially in the more challenging early stage cases.
Umeoka, Dr. Takashi Koyama, Dr. Ken Tamai et al preoperatively evaluated 51 esophageal lesions in 49 patients (ages 44-84, mean age 61.7, 42 men and 7 women) who subsequently underwent surgery for 47 squamous cell carcinomas, three adenocarcinomas, and one melanoma.
Following intravenous injection of 100 mL of nonionic contrast material (3 mL/sec), arterial- and venous-phase images were acquired at 35 and 65 after triggering of the ascending aorta at 1 x 8-mm collimation on an eight-slice scanner (Aquilion, Toshiba Medical Systems, Tokyo), Umeoka said.
Two GI-experienced radiologists evaluated the images in a blinded fashion for the presence, localization, and T staging of the tumors as follows, and the results compared with histology.
- Tx -- poorly visualized
- T1 -- focal enhancement along the inner wall of the esophagus without wall thickening
- T2 -- enhanced wall thickening with preserved outer muscle layer of less enhancement
- T3 -- enhanced wall thickening without preserved outer muscle layer
- T4 -- obliteration of the fat layer between the esophagus and other organs
The final pathological staging confirmed 17 T1 tumors (three T1a, 14 T1b), 10 T2, 20 T3, and four T4. In arterial-phase imaging, CT's accuracy was 64.7%, 25%, 85%, and 87.5% for stages T1, T2, T3, and T4, respectively. All three T1a tumors were classified Tx, while the other 48 tumors were clearly identified, Umeoka said. For venous-phase imaging, staging accuracy was 11.8%, 0%, 90%, and 87.5% for T1, T2, T3, and T4, respectively, with 13 stage T1 lesions rated Tx.
 |
| Arterial-phase image of 60-year-old male with T1b esophageal cancer. The tumor is clearly enhanced on the arterial phase (arrow). The lesion was T1b at surgery. All images courtesy of Dr. Shigeaki Umeoka. |
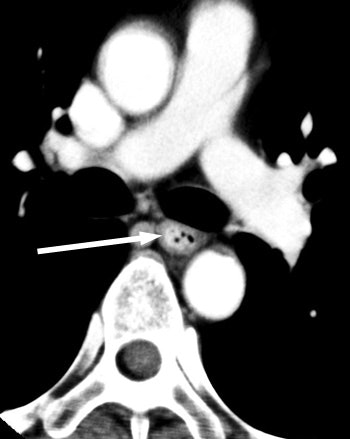 |
| Venous-phase image of a 60-year-old male with stage T1b esophageal cancer. The tumor cannot be seen in the venous phase. |
"Regarding overall accuracy, arterial-phase images were superior to venous-phase images 65% versus 43%," Umeoka said. "Especially, the arterial-phase images can improve the accuracy of T1b cancer staging, 78% versus 14% (on venous phase), and arterial-phase imaging correctly diagnosed all but three stage T1 cancers." Still, "most T2 cancers were overdiagnosed as T3 cancers ... because the preserved muscle layer was too thin to demonstrate," he said. Accuracy for stage T3 and T4 cancers was similar between the arterial phase and venous phase images.
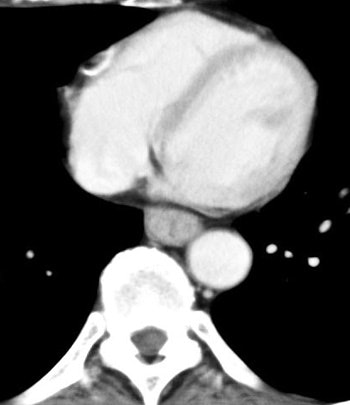 |
| The arterial phase image of 64-year-old male with T3 esophageal cancer. In this case, the tumor is visualized as "wall thickening." The muscle layer cannot be seen. |
 |
| Venous-phase image of 64-year-old male with T3 esophageal cancer. On this phase, the tumor can be seen as well. |
"Our results show several advantages for arterial-phase imaging," Umeoka said. "Arterial-phase imaging improves overall accuracy, especially T1b and T2 cancers, due to improved conspicuity. Most T1b cancers can be diagnosed only in the arterial phase. Exact localization may also be necessary for planning radiation therapy or surgery."
Ultrasound is still the best modality for local staging, he said in response to a question from the audience.
Better staging in a heartbeat
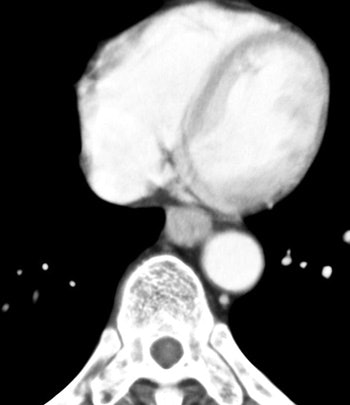
In another RSNA presentation, Dr. Kiyohiko Shuto and colleagues from the Graduate School of Medicine at Chiba University tested a novel method of evaluating pericardial invasion in advanced esophageal cancer.
"It is important to diagnose preoperatively whether the tumor invades the (esophageal) adventitia or adjacent structures such as the tracheal bronchus or left atrium because a curative operation is impossible for these T4 cancers," Shuto said. "Pericardial invasion, especially of the left atrium, can be difficult to evaluate because of pulsation artifacts on conventional CT."
Shuto, whose team included Dr. Nobusada Funabashi and Noriyuki Yanagawa, sought to reduce the effects of motion artifacts in their study, which evaluated 12 patients who were diagnosed with esophageal cancer. The group performed contrast-enhanced ECG-gated CT on a LightSpeed 16 scanner (GE Healthcare, Waukesha, WI), using 1.25-mm slice thickness, pitch 6, 30 seconds after injecting 100 mL of iodinated contrast at 350 mgI/mL.
The images were reconstructed at every 10% of the RR interval from 0% to 90%, with the data transferred to a workstation. "Images were compared histologically after esophagectomy," Shuto said.
"In the atrial contraction period, we could observe a low-density band between the left atrium and the (esophageal cancer), but it was undetectable in the end-systolic phase," he said. "The low-density band between the (left atrium) and the (esophageal cancer) in the 70% to 80% portions of the RR interval could be visualized in all 12 subjects; however, it was not visualized in the 40% portion in any of the subjects."
A 4D movie of a reconstructed dataset revealed further details.
"The left atrium contracts separately from the esophageal cancer, and we concluded that the tumor does not invade the left atrium," Shuto said. "(The case was) diagnosed as T3. All 12 subjects underwent esophagectomy, and all revealed squamous cell carcinomas. No one had evidence of esophageal cancer invasion of the left atrium in histological findings."
Thus, the negative predictive value was 100% for identifying pericardial invasion. "We predicted if a low-density band between left atrium and the esophageal cancer is visualized, the tumor will be stage T3 cancer.... ECG-gated multislice CT can reduce the influence of cardiac pulsation," he concluded.
ECG-gated multislice CT is potentially very useful for evaluating pericardial invasion of esophageal cancer, Shuto said. It is very difficult to assess pericardial invasion using ultrasound, he added in response to a question from the audience.
By Eric Barnes
AuntMinnie.com staff writer
February 28, 2005
Related Reading
PET improves on CT in staging esophageal cancer, February 3, 2005
U.S. cancer survival rates rising - report, January 20, 3005
Sharp rise in esophageal cancer rates reflects increased disease burden, January 20, 2005
FDG-PET sensitive for assessing esophageal cancer, June 21, 2004
Esophageal cancer treatment keeps pace with technology, July 21, 2003
Copyright © 2005 AuntMinnie.com




















