VIENNA - A key difference between colorectal cancer and other malignancies is its generally slow pace of development. Its engine, the so-called adenoma-carcinoma sequence, nearly always unfolds over years or even decades, making periodic colorectal cancer screening possible.
Lesion size is another crucial distinction. The largest colorectal polyps are far likelier to harbor cancer than the smaller ones. As a result, the correct categorization of polyp size at virtual colonoscopy is crucial to sound patient management.
However, a multicenter study that tested three reader groups -- VC experts, trained radiologists, and radiographic technicians -- found wide variations between endoscopically and radiologically reported lesion sizes, and only subtle differences among the three groups in their ability to categorize lesions on VC software.
Certainly the nine gastroenterologists in seven separate practices that measured excised colorectal lesions with forceps as histologic proof might have done their part to skew the overall assessment of lesion sizes. One might also argue that a little VC training goes a long way -- maybe the 50 cases given to the nonexpert groups put them nearly on par with the pros.
In any case the study, based on data from a European Society of Gastrointestinal and Abdominal Radiology (ESGAR) trial, did conclude that experience makes a positive and measurable difference in performance.
"We know that the biological significance of colorectal adenomas depends on the amount of villous histology, the degree of dysplasia, but most important for (VC) on the maximum polyp diameter, such that approximately 1% of small polyps harbor malignancy, 10% of large polyps, and 30% to 50% approximately 2 cm in diameter or more," said Dr. David Burling from London's St. Mark's Hospital, who presented the results at the 2005 European Congress of Radiology.
"Polyp measurement is important because it places that polyp into a certain risk category," he said. "It's generally accepted that diminutive polyps 5 mm and smaller can be ignored. Patients harboring polyps 6-9 mm in diameter should be placed into a surveillance program, and those with polyps larger than 10 mm should be referred for colonoscopic removal."
But polyps are hard to measure, both radiologically and endoscopically. In VC, flat polyps are particularly challenging, and whether the lesion is seen in 2D or 3D, in soft-tissue or abdominal windows, can also make a difference, he said. Then there is observer experience.
In the study, Burling and his colleague Dr. Steve Halligan used the ESGAR trial data to measure the performance of 28 observers, including three groups of nine experts, nine radiologists, and 10 technicians. The expert readers had extensive VC experience, and each measured performance in line with published studies, Burling said. Nonexperts had minimal or no VC experience, but had been trained on 50 endoscopically validated cases. Each observer categorized the cases according to the largest lesion seen, including cancer, large polyp (10 mm and larger) and small polyp (6-9 mm). Polyps smaller than 6 mm were deemed normal.
VC was performed in a standard way using multidetector-row CT on 51 patients from the participating centers, all of whom had tested positive for fecal occult blood. There was no IV contrast or fecal tagging. The cases were defined by the largest lesion at colonoscopy, as determined by measurement at polypectomy using forceps.
"When (the observers) found a polyp, they placed a computer software compass (Voxar Colonscreen 2.2, Barco, Kortrijk, Belgium) across the maximal dimension they perceived on any of the 2D planes -- not the 3D," then categorized the polyp based on the above criteria, he said.
According to the endoscopically validated results, 375 (283 large and 92 small) polyps were read by 28 observers, of which 167 (45%) were detected. There were 12 large polyps 10-40 mm in diameter, four small polyps 7-8 mm, and the smaller lesions not counted on the radiology side.
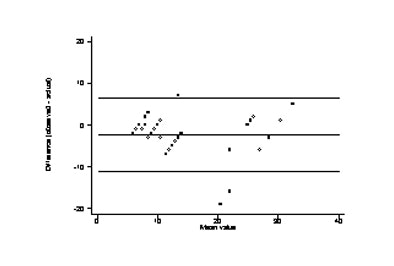
For large and small polyps, the mean difference between the radiologic observers' measurements and the endoscopists' reference size was -2.1 mm for experts (95% Bland-Altman limits of agreement, -9.4 to 5.2), -2.8 mm for radiologists (95% limits of agreement, -13.3 to 7.7), and -2.2 mm for radiographic technicians (95% limits of agreement, -11.1 to 6.6).
"You can see that the difference between (VC) and colonoscopy was generally underestimated," Burling said. VC "generally underestimated the colonoscopy value by 2-3 mm," he said. "Also important are the Bland-Altman limits, between which 95% of measurements will fall. For example, a radiologist might be mismeasuring by up to 13 mm less than the true value. Displayed graphically (below) you can see the limits are quite wide, but narrower for the experts (below left) compared to the either the radiologists or the radiographic technicians."
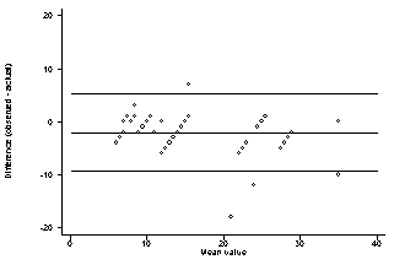 |
| Bland-Altman test of variation between polyp size measurements among VC experts (above) versus trained radiologists (below) and radiologic technologists (bottom) demonstrates slightly less variation among experts. Charts courtesy of Dr. David Burling. |
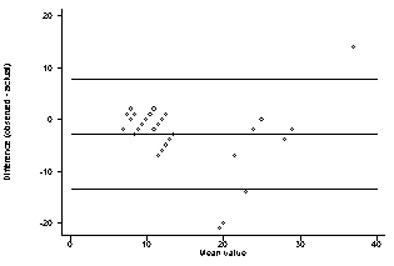 |
 |
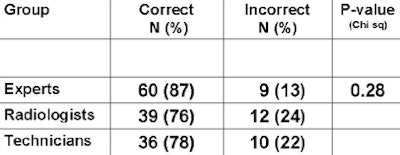
The median difference in absolute measurement variability was the same for all three observer groups, although there was a statistically insignificant trend toward experts' measuring a little more accurately (p = 0.39). As for categorization accuracy (chart below), of the 16 polyps cases six were very difficult to detect, with only one expert seeing two of the polyps. All observers correctly categorized three very large polyps. Of the seven miscategorized polyps, six measured 10-15 mm, close to the important size management threshold, and all observers overestimated one 7-mm polyp, he said.
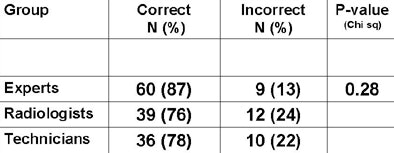 |
| Expert readers showed a trend toward better lesion categorization in chi-squared statistics, but the differences did not reach statistical significance (p = 0.28). |
Overall experts saw more polyps than nonexperts, and there was a trend toward the experts' categorizing polyps more accuracy (p = 0.28). But overall the study observers underestimated polyp size, Burling concluded. Limitations included the potentially significant variability of size measurements reported by nine gastroenterologists in seven practices. In colonoscopy there was also a spectrum bias toward large polyp size, and the VC software permitted only 2D measurements, he said.
"We could conclude from this study that you don't need a great deal of experience, (but that) experts probably categorize (polyps) more accurately," he said. Training, he added, "is key to bringing up performance."
By Eric Barnes
AuntMinnie.com staff writer
March 8, 2005
Related Reading
Training key to VC performance, but how much is anyone's guess, February 8, 2005
CAD for VC improves reader performance, sensitivity for larger polyps, May 18, 2004
VC researchers push for study quality, consistency, March 17, 2004
Experience sharpens role of IV contrast-enhanced VC, January 19, 2004
Copyright © 2005 AuntMinnie.com