Researchers from the University of Munich in Germany produced two studies that put 16-slice MDCT to the test for detecting musculoskeletal tumors. In the first, MRI was far more sensitive than CT for detecting spinal metastases, as it could see early soft-tissue changes in the bone marrow before the onset of bone damage.
However, a second study by mostly the same research team found that ultralow-dose CT detected 100% of the osteolytic lesions detected at both standard-dose CT and MRI. Moreover, CT was faster and cheaper than MRI, and more accurate than the standard radiographic workup the hospital had been using.
MRI for spinal metastases
In their study, Dr. Andrea Baur-Melnyk and colleagues from the University of Munich Grosshadern compared the diagnostic accuracy of high-resolution MR and MDCT for detecting spinal metastases in 41 patients (782 vertebral bodies) with various histologically proven primary malignancies.
CT images were acquired on a 16-row scanner (Sensation 16, Siemens Medical Solutions, Erlangen, Germany) at 120 kVp, 250 mAs, and 0.75-mm collimation. They were reconstructed using 3-mm overlapping slices, and multiplanar reformatted (MPR) reconstructions of the spine were also generated, Baur-Melnyk reported at the 2005 European Congress of Radiology (ECR) in Vienna.
Within three to four weeks, high-resolution MR images were also acquired on a 1.5-tesla scanner (Magnetom Symphony/Sonata, Siemens Medical Solutions). T1-weighted spin-echo images were acquired both pre- and postcontrast, followed by STIR images and T2-weighted spin-echo images, Baur-Melnyk said. All results were determined by consensus of two experienced radiologists.
 |
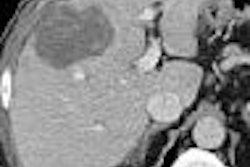
| In a 67-year-old woman with breast cancer, thoracic vertebrae 5-12 are displayed. No alterations of the osseous structures were detected on MDCT (left), whereas on MR STIR images (middle) the hyperintense signal in thoracic vertebrae 8, 11, and 12 depicted the bone marrow infiltration. A corresponding low-signal intensity on T1-weighted spin-echo images was also seen (right). Images courtesy of Dr. Andrea Baur-Melnyk. |
"In multislice CT, all osteolytic or osteoblastic metastases larger than 6 mm were reported," she said. "The gold standard cannot always be of course the histology in those patients. In some patients we had histology, but in the others we had to do an expert panel reading of both methods together from MRI and CT, or a combination of both methods."
The results showed that 424 lesions were deemed to be metastases in 782 vertebral structures. MRI had four false-negatives, but no false-positives, for an overall sensitivity of 99% and diagnostic accuracy of 99%. MDCT was less successful, calling 195/424 metastases "normal," and yielding four false-positive lesions, for an overall sensitivity of 55%, specificity of 98%, and diagnostic accuracy of 75%, Baur-Melnyk said.
"Sixteen-row multislice CT allows for thin collimation and high-resolution display of bony structures, but it is still inferior to MRI for the detection of (spinal) metastases," Baur-Melnyk said. "This is due to the direct visualization of the bone marrow (in MRI) before visually detectable osteoplastic or osteoblastic changes occur."
Equivalent detection in MRI, low- and standard-dose CT
Radiography plays a key role in the initial staging of multiple myeloma patients, who are typically followed up with MRI. But in a second ECR study by the Grosshadern team, Drs. Sonja Buhman, Andrea Baur-Melnyk, Maximilian Reiser, and Andreas Weiser found 16-slice MDCT to be a robust alternative to radiography for the initial workup of these patients, and even low-dose CT performed as well as MRI for detecting lesions.
"As all of you know, multiple myeloma represents neoplasia of the bone marrow as a member of the non-Hodgkin's lymphoma family," Buhman said in her presentation. "This neoplasia leaves a focal infiltration of the bone marrow and in most cases ends in osteal destruction -- mainly of the pelvis in this slide. Definition of the extension of osteolytic lesions, as well as of the fracture risk, is of great importance for correctly performed and adequate staging, which is necessary to be able to choose between several therapeutic options."
MRI is the gold standard for depicting multiple myeloma, as it provides excellent soft-tissue contrast and direct visualization of the bone marrow that is not possible with CT. But the team believed that CT might be preferable to x-ray if a low-dose CT protocol could do the job more effectively than radiography, and with a comparable radiation dose, she said.
The study examined 28 patients with confirmed multiple myeloma who were randomly assigned to one of two groups: group A, which underwent whole-body MDCT at 50 mAs; or group B, scanned at 100 mAs. All other settings (120 kVp, 0.75-mm collimation, and bone kernel) were the same for both groups. All images were reconstructed axially using 3-mm slices, and in the spine, sagittal reformats were also generated.
All patients had a whole-body MRI exam as well, on a 1.5-tesla Siemens Symphony scanner. The radiologists acquired coronal/sagittal STIR and unenhanced T1-weighted STIR-echo images.
The 50- and 100-mAs MDCT images were evaluated and graded subjectively by two experienced radiologists on a scale of 1-4, 1 being excellent. ROI measurements (signal-to-noise plus contrast-to-noise ratio) and dose-length product was calculated for all the 50- and 100-mAs exams.
Mean image noise (24 HU) was far higher for the low-dose MDCT images (group A) than in the standard-dose 100-mAs images (12 HU) in group B, according to the results. Still, subjective image quality was rated excellent for both groups, and the radiation dose was far higher for the 100-mAs standard-protocol patients (men 3.7 mSv, women 3.9 mSv) compared to the 50-mAs group (men 1.85 mSv, women 1.95 mSv). The average x-ray dose was 4 mSv.
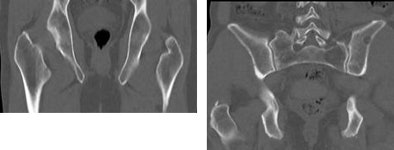 |
| Thin-section whole-body MDCT in a low-dose 50 mAs protocol (41-year-old male, right) performed as well as a standard 100 mAs protocol (54-year-old male, left) for detecting osteolytic lesions. Mean image noise (24 HU) was higher for the low-dose images (12 HU), but image quality was rated excellent for both groups, and the radiation dose was far lower in the 50 mAs protocol. Images courtesy of Dr. Sonja Buhmann. |
The average cost of the CT exam (320 euros) fell between that of radiography (230 euros) and MRI (590 euros). While MRI is the gold standard, CT offers high-resolution imaging and display of the trabecular structure. The CT exam was also faster, and perhaps most important, CT picked up every lesion detected by MRI, Buhman said.
"All osteolytic lesions that were primarily detected on the gold-standard MRI were also detected using 50 mAs as well as 100 mAs CT," she said. Considering the accuracy and the low effective radiation dose, Buhman said, it may be advisable to choose low-dose CT in favor of radiography for initial skeletal assessment in patients with multiple myeloma. Even at 50 mAs, CT still provided good image quality.
Spinal metastases throw different MRI signal intensities
Not all MRI-detected bone metastases are created equal. In another study presented at ECR, Dr. Joon Bum Koo and colleagues from Sangye Paik Hospital and the Inje University College of Medicine in Seoul, South Korea, retrospectively examined images of 106 patients with spinal metastases. On T1-weighted MR images, spinal metastases resulting from primary hepatocellular carcinoma (n = 23) yielded significantly higher signal intensities than those detected in patients with lung (n = 31), breast (n = 20), and GI tract primary malignancies (n = 18), as well as multiple myeloma (n = 14) (p = 0.00, one-way ANOVA test), the group reported.
By Eric Barnes
AuntMinnie.com staff writer
May 20, 2005
Related Reading
Cryoablation provides effect palliation for bone metastasis, April 4, 2005
MDCT staging may obviate bone scintigraphy in some patients, March 6, 2005
Bisphosphonates reduce skeletal morbidity of metastatic cancer, September 1, 2003
Single-fraction radiotherapy effectively treats painful bone metastases, October 10, 2003
PET useful for staging pediatric bone sarcomas, February 7, 2003
Copyright © 2005 AuntMinnie.com