For acute ischemic stroke, the CT sign of brain swelling without concomitant parenchymal hypoattenuation is no reason to exclude thrombolytic therapy based on the one-third rule, according to researchers from Seoul, South Korea.
The one-third rule is commonly used as the exclusion criterion for thrombolytic therapy in patients within six hours of symptom onset, and refers to the presence of early ischemic changes on unenhanced CT scans obtained in one-third or more of the middle cerebral artery territory.
While the early ischemic change of parenchymal hypoattenuation indicates severe ischemic edema of brain tissue and irreversible ischemic injury, the prognostic importance of a CT sign of brain swelling without concomitant hypoattenuation is questionable, the researchers stated in their study published in Radiology (June 2005, Vol. 235:3, pp. 992-948).
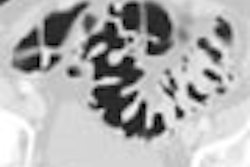
The researchers are from the Seoul National University College of Medicine, Seoul National University Hospital, and Samsung Medical Center, Sungkyunkwan University School of Medicine. The group hypothesized that brain swelling without hypoattenuation may not represent severe ischemic change. In a retrospective study of 14 patients, the team evaluated CT attenuation, apparent diffusion coefficient (ADC) on MR images, and perfusion parameters of lesions showing brain swelling without concomitant parenchymal hypoattenuation on CT.
The researchers found that the lesions with this CT sign had no cytotoxic edema and no significant decrease of ADC. The lesions had high relative cerebral blood volume (CBV), a mild to moderate time-to-peak (TTP) delay, and no significant relative cerebral blood flow (CBF) reduction.
Follow-up CT and MR images showed the lesions were normal in five cases, progressed to partial infarctions in six cases, and were complete infarctions in three cases. Occlusion of the proximal cerebral artery was found in all patients on MR angiography or conventional angiography.
"The mean time to CT and MR imaging ± standard deviation was 2.8 hours ± 1.5 and 5.2 hours ± 1.8, respectively, after symptom onset. The mean interval between initial CT and MR imaging was 2.4 hours ± 0.9, and the mean time to follow-up imaging was 5.7 days ± 1.6. The initial National Institutes of Health Stroke Scale score was 15.0 ± 5.6," the researchers wrote.
CT was done on a HiSpeed Advantage or LightSpeed Ultra helical CT scanner (GE Healthcare, Waukesha, WI), and MR imaging on a GE Signa or CV/i 1.5-tesla unit with echo-planar imaging sequences, including diffusion-weighted and perfusion-weighted imaging.
The region of interest (ROI) drawn for the gray matter of the lesion showing gyral swelling without hypoattenuation and the ROI drawn for the subcortical white matter of the lesion were compared with the mirror ROI drawn for the gray and white matter of the contralateral hemisphere.
The relative ratios of ADC, signal intensity on diffusion-weighted images, relative CBV, and relative CBF of gray and white matter were calculated by dividing the lesion values by the mirror ROI value of the contralateral hemisphere. TTP delay was defined as the difference between the TTP of a lesion and that of the contralateral hemisphere.
The values were compared with those of the contralateral hemisphere using a paired t test. The perfusion parameters of the three categories of lesions -- those that did not progress to infarctions, those that progressed to partial infarctions, and those that progressed to complete infarctions -- were compared using the Kruskal-Wallis test.
"The ADC of lesions was similar to that of contralateral normal tissue (p > 0.05). Lesions had an increased relative CBV (p < 0.001), a mild to moderate TTP delay (p < 0.001), and a variable but not statistically significant reduction of relative CBF," the researchers wrote.
"The mean relative CBF of gray matter was less in patients who had complete infarction (0.81 ± 0.16) than that in patients with partial infarction (0.99 ± 0.16) or those with a normal radiologic outcome (1.12 ± 0.22), but this difference was not statistically significant (p > 0.05)." they added.
Cerebral hyperemia
Brain swelling can be either due to cerebral hyperemia caused by increased CBV or due to cerebral edema caused by increased tissue water. Parenchymal hypoattenuation seen on CT in cerebral edema is related to the amount of tissue water content. A 1% increase in tissue water causes a decrease of 2-3 HU in attenuation on CT scans, stated the authors, citing a study in the American Journal of Neuroradiology (July-August 1998, Vol. 9:4, pp. 687-691).
Thus the CT attenuation of brain swelling caused by ischemic edema will decrease, but the CT attenuation of brain swelling due to cerebral hyperemia does not decrease, the group reasoned. "Our study suggests that brain swelling without hypoattenuation is predominantly caused by cerebral hyperemia and not by ischemic edema," they stated.
Based on published literature, the researchers also concluded a moderate TTP delay of less than six to eight seconds of the lesion with a CT sign of only gyral swelling may be consistent with TTP delay of oligemic or penumbral tissue.
"This CT sign of early ischemic change does not represent severe ischemic damage, but it does suggest ischemic penumbral or oligemic tissue," they wrote.
By N. Shivapriya
AuntMinnie.com contributing writer
May 26, 2005
Related Reading
Radiology residents can accurately evaluate after-hours head CTs for stroke, May 20, 2005
Beyond CT: Diagnosing the unusual stroke, October 20, 2004
MR vs. CT? Stroke imaging hinges on more than modality, August 25, 2004
Perfusion CT predicts, measures, thrombolysis benefit after acute stroke, December 24, 2003
Perfusion CT offers speedy access, but MRI gives the "big" picture, February 19, 2003
Copyright © 2005 AuntMinnie.com