AuntMinnie.com is pleased to present the first installment of our two-part series on building a community-based CT angiography practice in an imaging center, based on discussions by radiologist Dr. David Dowe of Atlantic Medical Imaging in Galloway, NJ. Part I covers workflow and patient selection.
Time is not only money -- patient satisfaction is also linked to faster exams in the community-based MDCT practice. Workflow issues are critical to the bottom line, and proper patient selection can spell the difference between success and failure, according to radiologist Dr. David Dowe.
Choosing patients wisely and minimizing table time not only keeps patients happy, it can prevent failed exams and a whole range of avoidable complications, said Dowe, a radiologist and proprietor of Atlantic Medical Imaging in Galloway, NJ.
Whom to scan
"Proper patient selection saves time -- don't be your own worst enemy," Dowe said in a presentation at last month's International Symposium on Multidetector-Row CT in San Francisco. "You should know by now who's going to be successful in your scanner for coronary CTA."
High on Dowe's list of don'ts are patients with atrial fibrillation, bigeminy, trigeminy, and of course, high-grade heart blockages.
"Atrial fib is a big one," he said. "I do attempt atrial fib here and there, and if the overall (heart) rate is sub 80 I'll give it a shot. I've had some success on the 16-slice (scanner) as well as the 64-slice, but doing atrial fib relies on a lot more luck than skill."
Bigeminy and trigeminy are absolute contraindications, but may not be so in the future, when it will be possible to edit the ECG tracing, Dowe said. High-grade heart blockages preclude beta blocker administration. Severe asthma can be a tough call for cardiac CTA, but most asthmatics can tolerate a single dose of oral beta blocker. Others may do better with calcium channel blockers, he said.
"What I always do with asthmatics is consult with their private physicians to ask them permission to give beta blockers," Dowe said.
Don't perform coronary CTA on patients with renal insufficiency (creatinine > 1.8), or on patients with pacemakers, in which artifacts are the main problem.
"You get the lead stuck up in the right atrial appendage, and you're not going to get the proximal vessels, and if you're not going to get the proximal vessels, there's no need to do a coronary CTA," Dowe said.
The traditional contraindication of morbid obesity becomes less of a problem every year, with MDCT scanners putting out higher and higher mAs, preventing photon starvation in such patients. A 64-slice MDCT scanner can yield mAs as high as 800 with a slice thickness of 0.625 mm, Dowe noted.
Finally, he said, don't scan patients with a failed steroid prep in the office setting. Such exams should be performed in a hospital, where anesthesia, or at least standby respiratory therapy, is available.
Speed patient prep
Most of the center's patients pick up a complete imaging packet the day before the exam, including a cardiac medical history form to fill out, a brief description of what to expect when having CTA, and their dose of oral beta blocker. The patient then takes the beta blocker before driving in for the exam, and arrives medicated.
"I've had zero beta blocker complications -- which totally amazes me," Dowe said.
Alternatively, patients who don't want to pick up the packet can arrive an hour early on the day of the exam. The center can also fax a prescription to the patient's pharmacy, or the patient's primary physician can supply the beta blocker. But 99% of Dow's patients pick up the packet the day before imaging, and the primary physician is not involved, he said.
Preauthorizing the insurance a day before the exam prevents another source of delay. At any rate, in New Jersey all coronary CTA exams must be precertified or preauthorized except in Medicare patients, he said.
Thus, "history forms are completed, the beta blocker is in their stomach, the insurance has been verified before they even get to the front door," Dowe said. Everybody gets beta blockers, and when vendors say they're not necessary on their 64-slice machines, they are stretching the truth, he said.
Ready, set, go
The patient's vital signs are obtained in a separate prep room. On the practice's 64-slice CT scanner (the only one used for coronary CTA), a heart rate of 70 bpm is the cutoff, and a second dose of beta blocker is given if the rate still exceeds 72 bpm.
"Nobody gets on the CT table without prior verification that their heart rate is as low as we can safely get it," Dowe said. Moreover, a low, steady heart rate enables single-sector image analysis, and 10-minute image reconstruction times. Finally, a low heart rate permits the use of dose modulation to reduce the radiation.
If oral beta blockers fail to slow the heart rate sufficiently, the practice has a separate room for the administration of IV beta blockers, but these are avoided whenever possible, he said.
"The reason I don't like to give IV beta blockers is that it ties up the scanner. Any time I look in the scanner room and I see a nurse, a tech, a patient, and the gantry's not spinning, I get chest pain," he quipped.
Not only do IV beta blockers necessitate more staff time, the commotion surrounding it works against the patient's obtaining a low heart rate. When the patient sees the staff administering an IV while watching the monitor, the patient is going to watch the monitor too. "It works against you," Dowe said.
After the scan the nurse pulls the contrast IV, the patient gets dressed, and 10 minutes later the radiologist is examining the images with the patient.
"Is there anything else in medicine that you get the results 10 minutes after the test? I have gotten surprisingly no push-back from the referring docs that I am giving the patients the results -- which shocked me," he said.
After the patient leaves, the exam is dictated, the technologist creates 3D virtual reality images, and the report is mailed to the referring physician.
"I guarantee that if you buy into (this method) and follow it, you will be successful," Dowe said. "Then if you're lucky you may get to experience one of life's little joys, which is making a cardiologist miserable."
By Eric Barnes
AuntMinnie.com staff writer
July 8, 2005
Coming up in Part II: Building the cardiac CT practice.
Related Reading
CT nips at MRI's heels in LV function study, June 29, 2005
Multislice CT reveals previous plaque rupture in coronaries, June 14, 2005
CTA seen as accurate complement to invasive angiography, May 24, 2005
Noncoronary findings often identified on CT coronary angiography, May 18, 2005
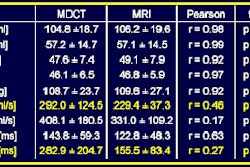
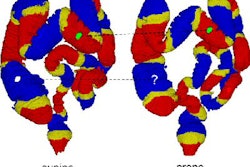
MDCT maybe equivalent to MRI, tops echo and SPECT for heart function, February 15, 2005
Copyright © 2005 AuntMinnie.com