
Imaging patients with built-in orthopedic hardware is a tough job almost by definition; most of the time artifacts cannot be eliminated completely in any modality. But scanning is a necessary evil for assessing healing of bony structures, and determining whether further intervention is needed.
Multidetector-row CT (MDCT) may do a better job than other modalities when it's performed carefully, according to musculoskeletal radiologist Dr. Garry Gold. As usual, success means careful planning.
"When considering scanning orthopedic hardware, you need to consider the amount of metal, its orientation in the gantry, the CT settings, and the type of metal," said Gold, who is an assistant professor of radiology at Stanford University in Stanford, CA. "Aluminum is by far the easiest to scan, and cobalt chrome as we see in hip replacements typically gets to be a little bit of a problem."
To maximize resolution, Gold's group follows the so-called "3-1-0.5" rule for its MDCT scans, meaning that maximum collimation is set at 3 mm in large sections such as the pelvis and shoulder girdle, 1 mm at the elbow and knee, and 0.5 mm for hand, wrist, and foot imaging.
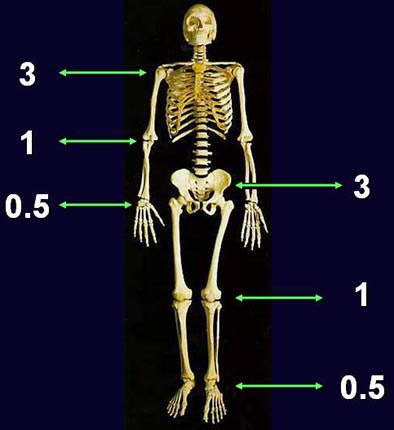 |
| For MDCT the traditional 3-2-1 rule is modified to 3-1-0.5, meaning that maximum collimation is set at 3 mm in large bones such as the pelvis and shoulder girdle, 1 mm for elbows and knees, and 0.5 mm for hands, wrists, and feet. All images courtesy of Dr. Garry Gold. |
"It used to be the 3-2-1 rule, but the technology keeps improving," Gold said in a presentation at the 2005 International Symposium on Multidetector-row CT in San Francisco. And beyond thinner slices, kVp and mAs should be adjusted upward, pitch reduced to less than 1, and scan orientation adjusted to minimize the x-rays hitting the metal, he said.
"You want to minimize the amount of metal in the scan plane to reduce beam-hardening artifacts," Gold said.
Typical voltage settings range from 120-140 kVp. Thick anatomy needs more mAs, and more metal requires higher mAs, he said. Even thin anatomy needs more mAs to maintain adequate signal-to-noise ratio, but little attenuation is needed in peripheral regions such as hands.
MDCT can even handle patients who have undergone total hip replacement (THR), though imperfectly. THR hardware typically contains larger amounts of denser metals than other applications, making diagnostic scans harder to produce, Gold said.
Still, Gold and colleagues' THR protocol works fairly well, he said. The group acquires data for both hips, using slices of 2-3 mm at 1-mm intervals, pitch under 1, 140 kVp, and a large focal spot. Soft-tissue filters are favored over the bone algorithm, multiplanar reconstructions (MPRs) of 2-3 mm are used for reading, and mAs can reach as high as 900, depending on the patient, he said. THR patients tend to be older, so there is less concern about dose.
In THR cases the reader is looking for bone stock loss, loosening, particle disease, or infection, Gold said. There is always some artifact from the acetabular components, which are typically cobalt chrome, but CT can render a diagnosis that is hard to make on plain radiography.
"Here we're looking at hip replacement with a lot of lucency around the acetabular component, as well as around this screw that's fixating the acetabular component on the sagittal MPR," he said, projecting an example on a screen. "This may end up to be infection or it could just be loosening. Just like radiography we can't distinguish between the two, but we can at least indicate to the surgeon that they probably need to go in in this case."
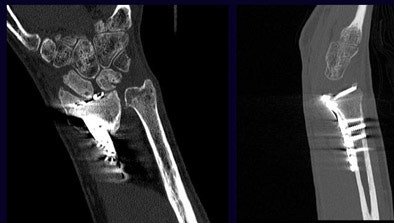 |
| Correct placement of the orthopedic plate and screws are investigated in wrist images. MDCT shows a cystic change and some widening of the scaphoid bone. It appears that at least two of the screws are in the radiocarpal joint, resulting in a recommendation that the orthopedic hardware be replaced. |
Another set of images showed a patient who had undergone open reduction and internal fixation of a hip fracture. New axial CT images showed a refracture through the proximal femur. In this case, the sagittal MPRs were very helpful for seeing a fracture that could not be seen on plain radiography, Gold said.
MDCT is also used to evaluate bony healing after orthopedic hardware is put in place. In a patient who had undergone a Fulkerson osteotomy for patellofemoral realignment, MDCT determined that bony union between the screwed-together tuburcle and underlying tibia had not yet been achieved.
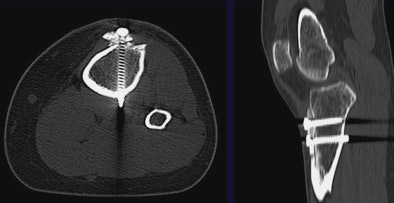 |
| MDCT can be used to evaluate bony healing following the placement of orthopedic hardware. The patient above underwent Fulkerson osteotomy for patellofemoral realignment. Two screws can be seen transversing the newly anteriorized tibial tubercle; however, bony union between the tuburcle and underlying tibia has not yet been achieved. |
And in a patient who had undergone both CT and MR arthrography, MDCT clearly showed the placement of a screw in the femur with respect to the articular surface and the patellofemoral joint, Gold said. The exact placement of the screw could not be determined in a corresponding MRI image acquired concurrently. In this case, he said, the CT image convinced the surgeon that further intervention was unnecessary.
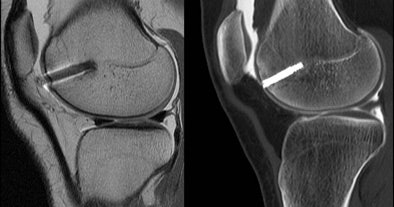 |
| CT arthrogram (right) shows placement of screw in the femur with respect to the articular surface and the patellofemoral joint. On MRI (left) the location of the screw relative to the bony cortex is difficult to pinpoint due to surrounding artifact. |
Having a PACS is very helpful for evaluating these cases, Gold said, because it allows the radiologist to benefit from two series of reconstructions: bone algorithm for MPRs and a soft-tissue algorithm for 3D reconstructions. Two-dimensional reformations are often preferred for diagnosis and evaluation, while 3D renderings are used mainly as a communication and surgical planning tool, he said.
"The orthopedic surgeons are sending us more of these cases all the time to evaluate for hardware complications," Gold said.
By Eric Barnes
AuntMinnie.com staff writer
October 26, 2005
Related Reading
MDCT, MRI competitive in some bone lesion applications, June 20, 2005
MRI sees spinal metastases earlier, but low-dose whole-body MDCT aces skeletal workup, May 20, 2005
MSCT beats x-ray in diagnosing TKA osteolysis, March 15, 2004
Copyright © 2005 AuntMinnie.com




















