
It isn't easy to track down a resected human colon specimen, tie it to a board, fill it with air for CT scanning, and painstakingly measure dozens of polyps with calipers for comparison with the imaging data. But it makes for a very realistic phantom experiment.
Dr. Stuart Taylor and colleagues from St. Mark's Hospital in London took the time to do all of these things, and in the process learned some interesting things about polyp measurement -- such as the finding that suboptimal colon distension doesn't seem to affect polyp size measurement per se, but does increase interobserver and intraobserver variability. The group also found that 2D and 3D each has a role in providing better accuracy under particular circumstances.
Polyp size measurements are critical in virtual colonoscopy because a few millimeters' difference can change patient management, from three-year surveillance to immediate polypectomy, for example. On the other hand, removing polyps that are too small incurs risks of bleeding and perforation with little chance of cancer prevention.
In a presentation at the International Symposium on Virtual Colonoscopy in Boston earlier this month, Taylor discussed the results of his group's study on polyp size measurement in virtual colonoscopy.
"The risk of malignancy as you know is dependent on the size of polyp, its histology, dysplasia, and shape. But when we're looking at CTC (CT colonography), all we've really got to look for is the size and maybe the shape, but we tend to go for the size as the main indicator," Taylor said.
The follow-up of polyps smaller than 1 cm is increasingly advocated, he said, but effective follow-up relies on accurate and reproducible measurements to determine if the polyp has grown in the follow-up period.
"But when the patient comes back for follow-up (VC) a year later, it may be a completely different bowel prep, it may be a different protocol, the amount of air in the colon may be different, the radiologist looking at the scan may be different, and there may even be different techniques where they measure the polyps in 2D or 3D," Taylor said.
The research team, which also included Dr. Andrew Slater, Lesley Honeyfield, Dr. David Burling, and Dr. Steve Halligan, aimed to investigate the effects of multiple variables including colonic distension, reader experience, and measurement technique on polyp size.
The phantom was a polyp-rich colon specimen from a patient with familial adenomatous polyposis who had undergone prophylactic colectomy to avert a future risk of colon cancer. The specimen was secured to a plastic board and submerged in saline. It was insufflated with the aid of a balloon catheter and suturing, and scanned twice on a multidetector-row CT scanner using 1.25-mm collimation, 1.5-mm reconstruction interval, and 50 mAs.
The first scan followed suboptimal insufflation of "about 20 puffs of air" applied manually, Taylor said (cecum < 5 mm). The second scan was with an optimally distended specimen, following about 40 puffs of room air (cecum > 5 mm).
The specimen was then opened and divided into 15-mm segments. With the aid of calipers, a histopathologist measured the maximum dimension of all polyps larger than 3 mm.
 |
| Human colectomy specimen above (below, close-up view of 15-mm section) was distended with air and imaged on CT. Polyp sizes measured on the 2D and 3D datasets were then compared with careful manual measurements performed with calipers. All images courtesy of Dr. Stuart Taylor. |
 |
"We took digital photos of each section, and some poor study coordinator, which was me, had to go through all these digital photographs to map these tiny polyps," Taylor said. "I took these close-up photos and (drew) maps between individual polyps to see how far it was between each polyp, and how far between the haustral folds and the ileocecal valve so I could find where the polyps were."
Then two observers, an experienced radiologist and a trained radiologic technologist, who were aware of polyp locations but not size, independently estimated the maximum polyp diameter in each dataset using software calipers on both 2D (choice of MPR, oblique, and windows) and 3D surface-shaded endoluminal views (Colonography 2, GE Healthcare, Chalfont St. Giles, U.K.). The readers, who were blinded to their previous measurements, were presented with the polyps in a randomized order, with 2D and 3D reads separated by at least a week's time.
In all, 21 polyps 3 mm or larger were available for analysis, Taylor said. Only one polyp was larger than 10 mm. The results showed 2D polyp measurements to be significantly smaller than their true histological size at half distension (radiologist: mean difference -1.1 mm sd 1.3, p < 0.001; mean difference, technologist: -1.7 mm sd 0.8, p < 0.001). At full distension the same measurements were -1.1 mm sd 1.3 p <0.001 for both readers.
The radiologist's 3D measurements were close to the true sizes for both the half-distended and the fully distended datasets, while the technologist's measurements were significantly smaller for both (half-distended mean difference: -0.7 mm sd 1.2, P=0.01; and full distension mean difference: -0.8 mm sd 1.5 mm, P=0.003).
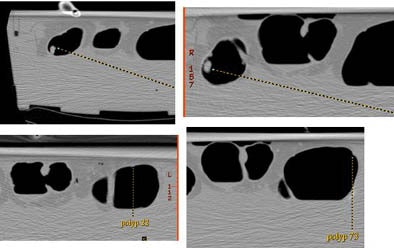 |
| Each of the 21 polyps in the specimen was matched and measured with the CT data, but at half distension (left) and full distension (right) on both 2D and 3D views. |
The combined observer Bland-Altman 95% limits of agreement were similar for both datasets (half distension: 2D -3.7 mm to 1.5 mm, 3D -2.9 to 1.6 mm; full distension: 2D -3.8 to 1.3 mm, 3D -2.9 to 2.8 mm).
"We can see that 3D is more accurate than 2D in the half distension, and similarly in the full distension 3D was more accurate than the 2D measurements," Taylor said. The technologist didn't do quite as well as the trained radiologist but the trends were the same, he added.
Good intraobserver agreement was found between the two datasets (expressed as the mean difference with 95% limits of agreement): expert 2D 0.1 mm (-1.8 to 2), 3D 0.6 mm (-2.5 to 3.8); novice 2D -0.4 mm (-2.1 to 1.2), 3D -0.4 mm (-2.8 to 2.7).
Intraobserver agreement is tested when the same reader measures the exact same polyp both at half and full distension, Taylor said. "The radiologist was more accurate -- agreement was better -- using 2D (rather) than 3D. Between half and full distension for some reason in 3D measurements the agreement became less. Same for the technologist -- (intraobserver) agreement was better using 2D than it was using 3D."
The results also appeared to show that experience improves reader accuracy, and that 3D is more accurate for absolute polyp size measurements than 2D, Taylor said.
"The degree of distension does not adversely affect the actual accuracy of polyp size measurement. However, what it does do is increase interobserver variation," he said, noting that suboptimal colon distension increases both interobserver and intraobserver variability, especially when viewed in 3D.
As a take-home point, "maybe we should say that if a patient comes back in three years' time and the colon is not as well distended as it was in the original scan, maybe we should be using 2D rather than 3D," Taylor said.
In response to audience questions, Taylor acknowledged that the applied 95% confidence limits could incorporate polyp size differences as large as 3 mm. Therefore, to be certain that a lesion had grown at follow-up, demonstrated growth would probably need to be greater than 3 mm. Differences in polyp morphology could also complicate size measurements, he said.
By Eric Barnes
AuntMinnie.com staff writer
November 4, 2005
Related Reading
Polyp measurements more accurate in 3D, September 6, 2005
VC experts have an edge over less experienced readers, March 8, 2005
Debate over 2D versus 3D VC reveals subtle differences, January 21, 2005
Copyright © 2005 AuntMinnie.com




















