By definition, symptomatic screening patients deserve the lowest possible CT dose. For that matter, "as low as reasonably achievable" (ALARA) is a wise dosing strategy for symptomatic heart patients, too. A look at the diagnostic question at hand and adherence to a few scanning principles can often reveal opportunities for significant dose savings, according to a recent presentation.
Cardiac imaging expert Dr. Joseph Schoepf discussed the most important methods for reducing the cardiac imaging dose in common heart imaging applications in a presentation at the 2005 International Symposium on Multidetector-Row CT in San Francisco.
Schoepf, who is an associate professor of radiology and director of CT research at the Medical University of South Carolina in Charleston, surveyed the clinical practicability of several dose-cutting strategies for calcium scoring, pediatric cardiovascular imaging, and CT angiography in adults.
Calcium scan reproducibility
Today most sites use retrospective ECG gating for calcium scoring simply because it yields better reproducibility when the patient comes back for a follow-up scan, Schoepf said. Beyond that, he said, dose modulation should be used for every patient's calcium scan.
"The number one application where you want to use ECG dose modulation for every patient is calcium scoring," he said. "It's a must in the a priori healthy population." Modulation brings the dose down to levels that are comparable to that of an electron beam scan or prospective ECG triggering with MDCT, Schoepf said.
Number two, very low dose settings can still provide high accuracy and reproducibility in calcium screening applications, Schoepf said.
In a study of 50 patients who were scanned twice with MDCT, Ohnesorge and colleagues showed that CT enables coronary calcium quantification with high reproducibility in follow-up exams using 3-mm overlapping increments compared with nonoverlapping increments. Minimum mean variability and minimum median variability with Agatston scoring were 12% and 9%, respectively, and 7.5% and 5%, respectively, with both volume and mass scoring methods (European Radiology, June 2002, Vol. 12:6, pp. 1532-1540).
A 2004 study by Schoepf's group showed that calcium scoring accuracy was not affected when mAs was reduced from 170 to 100 and even 50, though noise increased.
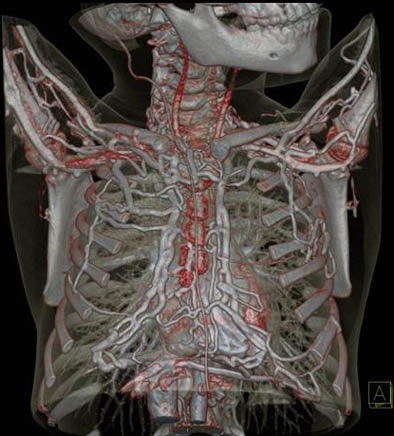
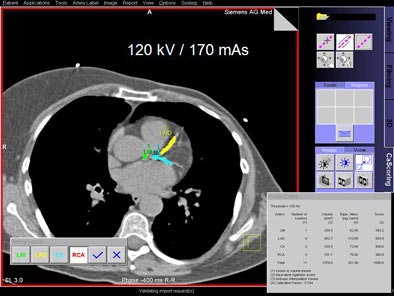 |
| Schoepf and colleagues found no significant differences in calcium scoring accuracy when mAs was reduced from 170 (above) to 50 (below). All images courtesy of Dr. Joseph Schoepf. |
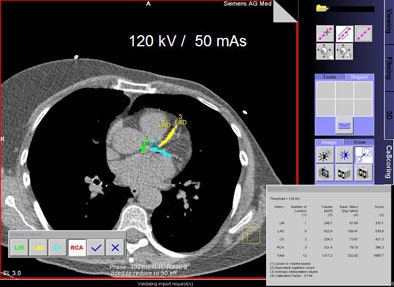 |
Comparing 170, 110, and 50 mAs in the same patient one finds "a lot of salt and pepper" noise at the low end, but if the calcium is measured using the mass score rather than the volume or Agatston scoring methods, the results are extremely accurate even at the lowest doses, Schoepf said.
"The combination of ECG modulation, low mAs, low kVp, and use of the mass score enables you to keep your radiation dose settings for coronary calcium scoring to the minimum," he said.
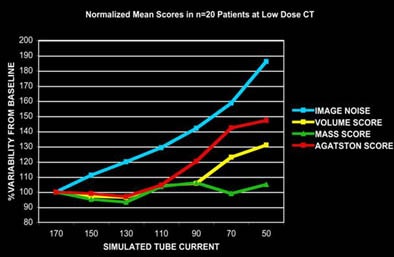 |
| A 2004 study by Schoepf and colleagues of normalized mean calcium scores showed that the mass scoring method was least affected by simulated tube current reductions in 20 patients. |
The pediatric heart
Cardiac CT in children gets a lot of attention these days, but the good news is that pediatric applications can be diagnostic at very low dose settings, Schoepf said.
First, weight-adapted algorithms should be used to determine the minimum mAs needed to answer the diagnostic question, and significant noise can often be tolerated, he said.
 |
| Congenital vena cava atresia is seen clearly at an ultralow 80-kVp, 44-mAs acquisition in a pediatric patient. |
Here automatic exposure control, which adapts the tube current to the precise portion of the anatomy being scanned, is the most important tool in the radiologist's arsenal, and should be used for every patient. "You can definitely and significantly decrease the radiation exposure in the pediatric population by using that," Schoepf said.
Keep in mind that pediatric cardiac CT needs to be "diagnostic, not pretty," he said. "Ask yourself if you really need ECG gating in your pediatric patients for congenital anomalies."
The answer is probably not. Instead use ECG pulsing, automated exposure control, and take advantage of the better x-ray absorption of iodine at low kVp settings, he said. This approach works equally well in slim adults.
CTA
ECG pulsing is the most important technique for reduced-dose CTA, Schoepf said. The technique, first published by Jacobs et al in 2002, takes advantage of the minimal motion for most patients in late diastole. At this moment (60% RR) the tube current is ramped up to 100%, then reduced to 20% during systole, when image data are unlikely to be used for reconstruction.
"You can save a whole lot of radiation dose if the patient -- and it has been stressed before -- has a slow and steady heart rate," Schoepf said. "Why does the heart rate have to be slow? The problem is that as the heart rate becomes faster, the part during systole when the tube current drops to 20% becomes smaller and smaller, so obviously the radiation dose savings that you can obtain by ECG pulsing are inversely related to heart rate."
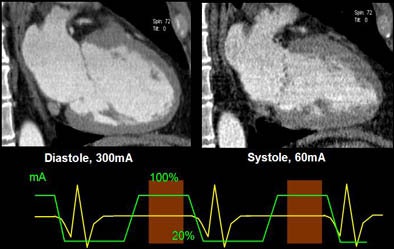 |
| Above, ECG pulsing reduces the mAs from 300 in late diastole to 60% in systole, cutting the overall radiation exposure significantly. Chart below shows that the dose savings achieved with ECG pulsing is significantly diminished as heart rate increases. |
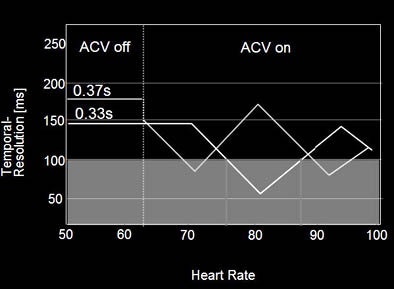 |
The rule of thumb is that ECG pulsing should be turned on if the heart rate is less than 65 bpm; most patients have a "sweet spot" around 60% RR. On the other hand, ECC pulsing should be turned off if the heart rate is greater than 65 bpm, because in these patients the sweet spot is less predictable, and is often found at around 30% RR.
To control heart rate, patients with heart rates greater than 70 bpm should be given a beta blocker such as 50-100 mg of oral metroprolol (Lopressor) 30 to 90 minutes before scanning (or 5-10 mg of IV metroprolol five to 10 minutes before scanning), provided there are no contraindications, he said.
At the same time, introduction of 64-slice scanners revealed the important observation that many patients, particularly those with faster heart rates, do not have their "sweet spot" or motionless period for image reconstruction during late diastole, but rather during late systole when the heart is fully contracted.
Even in a patient with heart rate of 125 bpm, reconstruction during the late systolic phase produced clear, crisp images with clear delineation of the cardiac tree on a 64-slice scanner, Schoepf said of an example.
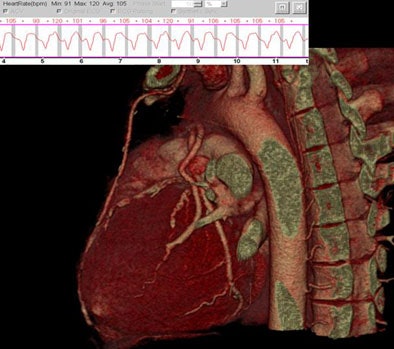 |
| In a patient with a rapid heartbeat of 125 bpm imaged on 64-detector MDCT, reconstruction during late systole produced clear images, albeit at a higher radiation dose. |
Still, late systole imaging is difficult, and not the lowest-dose option. "Slow heart rates are great," Schoepf said. "They give us broad acquisition windows, ample opportunities for ECG pulsing, (and) no need for multisegmental reconstruction. So rate control is not only important for image quality, it becomes a measure of radiation protection."
There are a number of strategies for dose reduction in clinical practice and they must be used whenever they're appropriate. "What kind of radiation exposure we give our patients is a make or break issue," Schoepf concluded.
By Eric Barnes
AuntMinnie.com staff writer
November 25, 2005
Related Reading
Coronary calcium screening seen useful beginning between age 40 and 50, September 23, 2005
Low-dose CT calcium scores near-equivalent of higher dose, September 20, 2005
Mass-based CT calcium scoring leaves room for dose reduction, April 30, 2004
Copyright © 2005 AuntMinnie.com