Researchers in California are hoping to revolutionize mammography quite literally -- with the aid of a prototype conebeam CT scanner that acquires images in a single revolution around the breast.
The scanner, code-named Bodega after a quiet town on the Northern California coast, performed comparably to mammography in a preliminary study of 21 patients and 10 healthy volunteers.
"This has never been done clinically," said lead clinical investigator Dr. Karen Lindfors in an interview with AuntMinnie.com. "The woman lies prone on the table and the breast comes down through a hole in the table, and the scanner makes one revolution around, in 16 seconds, and so it's not like a regular CT scanner."
The breast CT was developed and built in-house by University of California, Davis, radiology professor John Boone, Ph.D., in collaboration with Lindfors and Dr. J. Anthony Seibert, both from UC Davis, as well as Dr. Thomas R. Nelson from the University of California, San Diego. Funding was provided through $6 million in grants from the California Breast Cancer Research Program, the National Cancer Institute, and the National Institute for Biomedical Imaging and BioEngineering.
At the 2005 RSNA meeting in Chicago, Lindfors presented preliminary results from the first group of patients and control subjects, all of whom were imaged with the CT scanner as well as with regular two-view film-screen mammography.
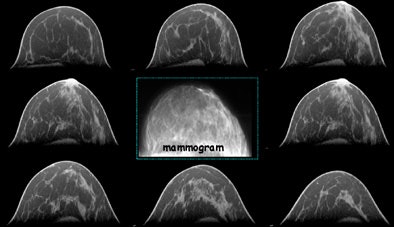 |
| Mammograms (above) and breast CT images (below) of a woman with biopsy-confirmed breast cancer. This patient has saline implants, which made the mammography detection challenging. The two views marked MLO (mediolateral oblique) and CC (craniocaudal) are the screening mammograms for this breast, and the other images along the top are the subsequent diagnostic workup images. The lesion is plainly seen in the three orthogonal breast CT images (arrows). In addition to visualization of the microcalcifications, the spiculated mass is seen well on the right-most CT image. Images courtesy of John Boone, Ph.D. |
 |
"We scanned 10 normal volunteers, then we scanned 21 patients who were BI-RADS 4 or 5 mammography patients who were going to have a biopsy, Lindfors told AuntMinnie.com. We scanned them before their biopsy, so we didn't know if the biopsy would be malignant or benign."
In a subjective, unblinded study that sought to compare the results of breast CT with standard two-view mammography, lesions detected on mammography were also seen on breast CT in 19 of the first 21 cases, Lindfors reported.
"One of (the lesions) was not imaged because the lady was really big-breasted, and anteriorly, where the calcifications were, wasn't imaged with the one scan that we did," she said.
The group hopes to solve that problem by building an adapter for use with large breasts that lifts the subject up off the table, permitting a second acquisition of the missed region. In the other patient with a lesion not seen in breast CT, the lesion was simply very subtle, Lindfors said. The missed lesions were histologically proven benign in both patients.
Another potential benefit of breast CT is comfort during the exam, which can translate into improved screening compliance. Unlike conventional mammography, CT of the pendulous breast requires no compression. So far patients seem to favor CT, Lindfors said.
"As far as comfort goes, we asked the patients about their position on the CT table, we asked them if they had difficulty holding their breath -- they had to hold breath for 17 seconds," she said. "We asked them about their overall comfort during the exam, we asked them about the comfort of breast CT compared to mammography."
On a scale of 1 to 10, 1 meaning mammography is far more comfortable and 10 meaning CT is far more comfortable, patients rated mean overall comfort at 5.4, thereby very slightly favoring CT, Lindfors said.
Advanced reconstructions are also possible, but are not typically needed to find the lesions, she said.
"I usually looked at them in the coronal, the sagittal, the axial planes, and I was able to do a 3D image but I didn't really look at that so much because I didn't find it helpful," Lindfors said. Interpretation is "a very real-time thing; it's ... a trackball and you scroll through the images," she said. "And of course we're refining all that because we're building the workstation too."
Nuts and bolts
On the engineering side is John Boone, Ph.D., a medical physicist who holds six scientific patents. His group built the scanner from scratch but for an off-the-shelf x-ray system, detector, motor, and the aid of a machine shop.
"How this differs from a regular CT scanner is that we don't have to penetrate the thorax because we have the woman lying pendant on the table, and the x-ray beam goes around in a horizontal plane and images the breast only," Boone told AuntMinnie.com. "Because we're imaging an average (breast) diameter of 14 cm instead of thorax, which is about 28 cm, we can reduce the radiation dose compared to a conventional CT scanner."
The images are acquired at 80 kVp, with an average of 73 mAs adjusted for breast size. "We have tuned the technique parameters kV and mA to give a woman exactly the same dose she would receive in two-view (mediolateral oblique and craniocaudal view) mammography," Boone said. For a standard-sized patient, the dose is on the order of 3 mGy x two views, or 6 mGy per breast. In terms of millisieverts, a typical absorbed dose of 5 mGy translates to 0.25 mSv, he said.
In another study presented at RSNA, Boone and colleagues calculated the modulation transfer function (MTF) by scanning a nickel-chromium wire, which produced a point-spread function in reconstructed images.
For the 500-projection image acquisition with a 512 x 512-mm reconstruction size, the MTF at a frequency of 0.5 mm dropped from 0.73 at the isocenter to 0.35 at a radius of 8 cm from the center, and similar trends were seen for other acquisitions and matrix sizes, the group reported in its RSNA abstract.
Thus, spatial resolution was highest at the isocenter, with very subtle image degradation at the image periphery, Boone said. The team is addressing this issue in its latest prototype scanner.
As for the clinical study, the results were subjective and only preliminary, of course. As soon as the group has completed exams in 200 patients with mammography and breast CT, they plan to submit the data to a blinded study read by two radiologists.
The researchers caution that it will take years to refine, optimize, and ultimately, they hope, change the way mammography exams are conducted. But they are optimistic that breast CT will ultimately bring real benefits to patients who need better screening options.
"We're not really interested in delivering the same performance as mammography or even digital mammography -- we're interested in delivering far superior performance, and this whole research project is focused on taking breast imaging to the next level," Boone said. "And while we have not proved it yet, we do think that breast CT will lead to earlier breast cancer detection in younger women and women with dense breasts. Certainly that is the group that will probably most benefit from breast CT," in the same way they have recently been shown to benefit from digital mammography, he said.
"There's great potential with CT," Lindfors said, "and at this point it's at least equivalent to mammography in terms of visualization. But again it's really preliminary data. I think it's going to be great but we have to wait a while before we really go crazy with it."
By Eric Barnes
AuntMinnie.com staff writer
December 20, 2005
Related Reading
MRI best for familial breast cancer detection, December 16, 2005
Dual-time-point breast PET increases diagnostic accuracy, December 2, 2005
Breast MRS proves sensitive to all cancers but not in normal breast tissue, November 27, 2005
Researchers make inroads with breast CT, gear up for clinical test, July 25, 2005
Copyright © 2005 AuntMinnie.com




















