
When it comes to assessing coronary calcium scores on MDCT, let the reader beware. Scores can vary widely based on the reconstruction interval, and the reconstruction with the least motion artifact -- not the highest score -- is likely the most accurate.
In a small series of patients, the "true" individual volume and Agatston scores were, in fact, distributed widely over the range of reconstruction intervals, German investigators reported at the 2005 RSNA meeting in Chicago.
Fortunately, the variability trended lower among patients with calcium scores over 100, but in some cases the differences were still sufficient to alter the patient's risk status according to German Cardiac Society guidelines. As a result, preliminary results of the ongoing study suggest the need to pay close attention to coronary calcium scoring techniques and results reporting.
"In the past decade it has been demonstrated that coronary calcification is an independent risk factor for coronary events, and a surrogate for coronary stenosis," said Dr. Jörg Barkhausen from University Hospital in Essen, Germany.
Until the advent of MDCT, the high cost of EBT scanners in Europe limited the number of facilities in which calcium scores could be assessed, he said. Scoring is gaining in popularity with the advent of MDCT, which relies on a different technique -- retrospective ECG gating -- to arrive at a calcium score. But the results have been highly variable.
Retrospective gating allows the reconstruction of different images "at different time points within the cardiac cycle," Barkhausen said. Thus, imaging quality and reproducibility with coronary calcium scoring are probably significantly influenced by motion artifacts.
The aim of the study was to compare the "real" calcium score as provided by the highest-quality reconstruction with the scores of other reconstructions over the entire cardiac cycle.
To that end, Barkhausen, along with lead investigator Dr. Peter Hunold and Drs. Thomas Schlosser, Ji-Sou Sawatzki, Axel Schmermund, and Hilmar Kühl, assessed coronary calcium retrospectively in 16 patients presenting with a clinical suspicion of coronary artery disease (12 men and four women; mean age 59 ± 9 years). Since presenting the data in November, the team has imaged approximately 35 additional patients.
Before CT each patient received beta-blocking medication (oral metoprolol or IV esmolol) and the resulting mean heart rate was 58 ± 6 bpm (range 46-67). The patients were imaged at 16 x 0.75-mm collimation on a 16-row scanner (Sensation 16, Siemens Medical Solutions, Erlangen, Germany) at 100 kVp, 80 mAs with a rotation speed of 420 msec, and 210-msec temporal resolution.
"Using a slice thickness of 3 mm and reconstruction increment of 2.5 mm, we performed 10 reconstructions in each phase through the cardiac cycle from -90% to 0% of the R-R interval," he said. Reconstructions were performed with Siemens' "CAscore" software, with Agatston as well as volume scores initially calculated for each individual vessel, then the total score for the entire coronary tree was calculated.
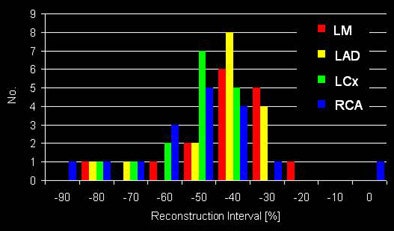 |
| Chart shows the optimal reconstruction interval for each artery. Within the range of -30% to -60 % of the R-R interval, 86% of the datasets had the best image quality. All images courtesy of Dr. Peter Hunold. |
The reconstruction with the least motion artifact by appearance was deemed the optimal reconstruction for each individual artery; the corresponding scores were considered the "real" scores. Total real scores (sum of individual optimum vessel scores) were compared to the range of scores from all different reconstructions.
"The total score was calculated according to guidelines of the German Cardiac Society, therefore the optimal reconstruction was used for the LAD (left anterior descending coronary artery), the RCA (right coronary artery), and the LCX (left circumflex artery), and then the sum of these scores was used as the total score," he said.
The "real" volume and Agatston scores obtained from the best individual reconstructions ranged from 0 to 811 and 0 to 924, respectively, Barkhausen said. The real calcium scores were distributed over the entire range of scores derived from different reconstructions.
The volume score was 51% ± 37% of the score range with a median of 53% and a range of 00% to 100%; the Agatston score was 53% ± 30% with a median of 58% and a range of 0% to 100%. A similar distribution across the entire range was seen when comparing real volume and Agatston scores with the ranges in the individual vessels. For individual vessels the optimal reconstruction intervals were: -30% or -40% in 11/15 patients and 12/15 patients for the left main and LAD, respectively; -40% and -50% (11/15 patients) for LCX; and -40%, -50%, and -60% (14/15 patients) for RCA.
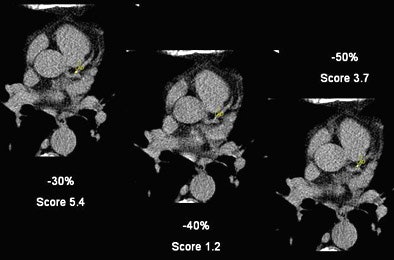 |
| A small calcification within the LAD shows the variability of calcium scores based on the reconstruction interval. The -30% reconstruction interval yields a calcium score of 5.4, a -40% reconstruction drops the score to 1.208, and at -50% reconstruction it is 3.7. |
"Comparing the two groups above and below (a score of) 100, the differences are more obvious for those patients with lower calcium scores," Barkhausen said. "Total score results are comparable for three different vessels, and we did see a wide range of different scores using different reconstruction intervals."
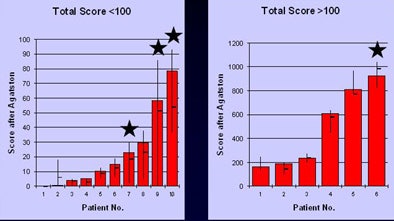 |
| Calcium score variability was more pronounced for patients with lower calcium scores, both in individual arteries and in overall results above. The stars indicate patients whose risk level was altered based on different reconstruction intervals. |
Even using a 16-slice CT scanner, the calcium scores were vulnerable to motion artifacts, Barkhausen said. "The optimal score obtained with minimum cardiac motion were not predictable and had to be evaluated in each patient. For each patient multiple reconstructions are necessary to get the true calcium scores, especially in those patients with minimal calcification," he said. "And the highest score is not necessarily the real score."
Without multiple reconstructions, variability is enough to impact the personal risk estimate for each patient, Barkhausen said. However, four reconstructions encompassing -30% to -60% of the R-R interval are sufficient to determine the optimal score.
In an e-mail to AuntMinnie.com, lead investigator Hunold noted that the initial results had been validated in approximately 50 patients imaged so far.
"It is absolutely clear that the conclusions (strongly differing scores depending on reconstruction) will be confirmed," he wrote. With regard to the new 64-slice scanners, he expects the variability to be lower but not eliminated.
"Since most of the 64-slice (scanners) have shorter rotation times compared to 16-slices, I suggest the variability will be lower," Hunold wrote. "I strongly believe that (variability) is not a matter of detector numbers."
By Eric Barnes
AuntMinnie.com staff writer
February 14, 2006
Related Reading
MDCT still can't differentiate between noncalcified plaques, January 10, 2006
Traditional risk factors may fail to identify women with atherosclerosis, December 19, 2005
Long-term anticoagulant users show elevated coronary, aortic calcium, December 2, 2005
Caution: U.S.A. may be hazardous to your health, October 3, 2005
Low-dose CT calcium scores near-equivalent of higher dose, September 20, 2005
Copyright © 2006 AuntMinnie.com




















