Multidetector-row CT is highly sensitive for identifying patients with degenerative aortic stenosis (AS), providing excellent correlation with transthoracic echocardiography (TTE) in quantifying disease extent, according to researchers from Austria.
"Degenerative aortic valve stenosis is the second most common cardiovascular disease and has an incidence of 2% to 7% in the Western European and North American populations over 65 years of age," wrote Drs. Gudrun Feuchtner, Wolfgang Dichtl, Guy Friedrich, and colleagues from the Innsbruck Medical University in Austria. "Patients with severe AS may require aortic valve surgery even when they are asymptomatic" (Journal of the American College of Cardiology, April 2006, Vol. 47:7, pp. 1410-1417).
The key to assessing AS severity lies in accurate measurement of the aortic valve area (AVA), with greater than 1.5 cm2 considered mild stenosis, 1-1.5 cm2 considered moderate, and less than 1 cm2 considered severe, according to American College of Cardiology and American Heart Association guidelines, the group wrote.
The team examined 46 patients (10 women, 36 men ages 45-78; mean age 69). Thirty patients had AS; 16 patients with known coronary artery disease were examined with MDCT and TTE prior to invasive coronary bypass surgery.
CT was performed on a 16-detector scanner (Sensation 16, Siemens Medical Solutions, Erlangen, Germany) using 12 x 0.75-mm collimation, table speed of 6.7 mm/sec, 120 kVp, and 300-450 mAs with radiation doses ranging from 6.7 to 13 mSv.
Transaxial images were reconstructed in increments of 0.6 mm, with the reconstruction window positioned in mid-to-late diastole corresponding to ejection phase in concordance with T-wave. The images, including left coronal oblique, left sagittal oblique, and other cross-sectional transversal levels, were analyzed on a Siemens Leonardo workstation using multiplanar reformatting (MPR) and volume-rendering techniques.
In 30 patients, TTE was conducted by an experienced observer using a Siemens Acuson Sequoia 256 scanner using a 3.5/1.75-mHz transducer. MDCT results were compared to TTE using the continuity equation with Doppler velocity-time integral for calculating aortic valve area.
According to the results, 30 of the 46 patients had AS as determined by TTE. MDCT detected 100% (30 of 30) patients with degenerative AS (95% CI, 88.3-100), with specificity of 93.7% (15 of 16). MDCT produced one false-positive.
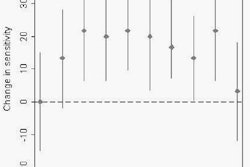
Linear regression analysis showed good correlation between AVA quantified by MDCT and TTE (r = 0.89; p < 0.001; 95% CI 0.78-0.95), the group stated. A Bland-Altman plot implied good intermodality concordance, with 27 of 30 patients falling within the limits of agreement (0.29; -0.20), while suggesting a slight overestimation of AVA (+0.04 cm2) by MDCT compared to TTE, the authors wrote.
Interobserver variability of AVA by MDCT was a mean 4.6%, while image quality graded on a five-point scale was rated excellent in 29 patients, good in 14, and mediocre in three.
Temporal resolution is sufficient (105-250 msec) with the use of a 16-detector-row scanner, fast rotation time (0.42 sec), and spatial resolution of 0.5 x 0.5 x 0.6 mm. In addition, the use of retrospective ECG gating permits image reconstruction at any time during the cardiac cycle and dynamic display of heart motion in cine CT, with reconstruction at every 10% of the RR interval.
TTE is widely used for the primary evaluation of AS; however, its potential limitations include difficulty in accurately measuring left ventricular outflow tract (LVOT) diameter and estimating the maximum velocity of the LVOT and aorta before flow acceleration, the authors wrote.
Moreover, other factors such as low cardiac output with aortic valve regurgitation, severe valvular calcification, or other unusual anatomic configurations can impair the echocardiographic window, limiting TTE results. Transesophageal echocardiography (TEE) can provide further evaluation; however, it is semi-invasive and must be implemented with great care in AS patients, the group stated.
As for MR's shortcomings, "slice tracking is not possible with two-dimensional cine CMR because the correct mid-to-end systolic position has to be identified in a longitudinal view in order to avoid being out of plane," they wrote.
On the other hand, the use of MDCT requires heart rate regularity, and the modality cannot be used to evaluate patients who are not in sinus rhythm. Heart rate should be below 80 beats/min to avoid motion artifacts, necessitating the use of beta-blockers in selected patients. However, extreme care must be taken when administering beta-blockers to AS patients.
MDCT is accurate and noninvasive method of identifying patients with AS, they concluded, cautioning that they "do not advocate (MDCT) as a primary diagnostic imaging technique in clinical practice because currently used TTE is accurate, safe, quick, and cost-effective."
MDCT makes a good alternative for patients in whom TTE is inadequate, and in those who undergo coronary CT angiography for the detection of concomitant and asymptomatic AS, they wrote.
Better with 64 detectors
In a follow-up conversation with AuntMinnie.com, the researchers explain the improvements that have come with the use of a 64-slice CT compared to the 16-detector machine in the study.
"Currently, we use a 64-slice CT scanner (Sensation Cardiac 64, Siemens Medical Solutions) instead of the 16-slice CT which clearly facilitates quantification of the aortic valve area," lead investigator Feuchtner wrote in an e-mail.
"We perform quantification of the aortic valve area in patients who are scanned for suspected coronary artery (disease) but who present with concomitant aortic valve calcification," she wrote. The comorbidity of coronary and aortic valve calcification is high because the pathomechanisms are similar.
The aortic valve area is a good parameter to decide whether an additional echocardiography is required for further follow-up of those patients, Feuchtner wrote.
"The vast majority of patients who have aortic valve calcification do not have aortic valve stenosis. But those who have aortic valve stenosis require echocardiography and close follow-up examinations, or may even require surgery although they are asymptomatic."
The new scanner offers a number of improvements over the 16-detector-row machine, including faster and easier postprocessing, she wrote.
With 16-detector MDCT, it took an average of three to five mid to late image reconstruction cycles to identify the phase of maximal aortic valve opening, Feuchtner wrote. In contrast, the 64-slice scanner comes with advanced software that automatically generates dynamic images (4D) during the entire cardiac cycle, facilitating the identification of the maximal aortic valve opening.
The group has performed approximately 350 cardiac CT scans utilizing 64-slice MDCT, creating aortic valve reconstructions in approximately 80 patients. Using 12% of the RR interval as the time point for image reconstruction is adequate in the vast majority of patients, and only one, or rarely two, image reconstruction cycles are needed.
Second, imaging at higher heart rates is improved as a result of better temporal resolution.
With regard to patient management, there is basically no difference between 16- and 64-detector MDCT regarding the clinical implementation in patients who are referred to coronary CTA and in whom aortic valve calcification are present.
In those patients, quantification of the aortic valve area can be used to detect or exclude aortic stenosis. If the aortic valve area is less than 2 cm², aortic stenosis must be suspected and the patient should be referred to transthoracic echocardiography.
MDCT is also well-suited for use in patients who require follow-up of aortic stenosis and in whom echocardiography is inadequate.
"There is one new clinical application regarding dynamic 4D cine imaging of the aortic valve in patients who undergo cardiac CT before aortic valve surgery for exclusion of coronary artery disease," Feuchtner wrote. "Dynamic 4D imaging may provide (important) information to the cardiac surgeon, e.g., if the valve commissures are partially fused or opened during systole; the presence, extent, and localization of valve and sinus valsalva calcification; and the valve morphology (bicuspid versus. tricuspid), which may influence the surgical technique -- surgical reconstruction versus aortic valve replacement."
By Eric Barnes
AuntMinnie.com staff writer
April 14, 2006
Related Reading
MDCT, MRI, TTE, TEE compared for aortic valve measurement, March 5, 2006
Multiple reconstructions needed for accurate MDCT calcium scoring, February 14, 2006
Doppler US accurate for spectrum of aortic valve measurements, January 26, 2006
Long-term anticoagulant users show elevated coronary, aortic calcium, December 2, 2005
Mitral annular calcification strong risk factor for stroke, December 2, 2005
Copyright © 2006 AuntMinnie.com