A soldier is wounded on a remote battlefield. Bleeding from a gunshot wound to a femoral artery, he is far from a field hospital where a complex operation might save his life. Blood pressure dropping fast, he slips from consciousness.
But this soldier is due for a high-tech stroke of luck. Rumbling onto the scene is an unmanned mobile ICU called the Trauma Pod. When it pulls up alongside him, a hatch door opens and a robotic stretcher scoops him up into its armored belly, quickly closing again.
A robotic surgeon, controlled by a human surgeon at a medical home base, oversees the patient as information is uploaded from sensors in the soldier's armor, garments, and even his smart dog tags. The patient is given oxygen, his vitals are assessed, and the robot begins stabilizing life-threatening injuries while communicating continuously with the manned base.
Then the patient is scanned from head to toe with CT, and the imaging data are automatically reconstructed and transmitted to the human surgeon.
 |
| Soldier is scanned with CT to determine nature of injuries. Image courtesy of SRI International. |
Within minutes the robot team completes its work. Tourniquets, gauze, and other supplies are dispensed from an automated tool kit. The bullet is extracted, an artery shunted, the wound is laser-welded back together.
The soldier's vital signs stabilized, he regains consciousness. An automated gurney rotates to an egress port on top of the vehicle and connects with a remotely piloted air ambulance for evacuation to the manned care facility.
Reality, not sci-fi
The Trauma Pod is not science fiction, but rather a working project of the U.S. Department of Defense that's well under way if not fully operational. The final version is expected to come online in approximately 15-20 years.
Here and now, the first phase of the project is taking shape based on existing technologies, all designed to be as open-ended as possible to facilitate their future evolution.
 |
 |
| Trauma Pod peacekeeping operations conceptual video, circa 2025. Video courtesy of the U.S. Defense Advanced Research Projects Agency (DARPA) and Dr. Richard Satava. |
A brainchild of the U.S. government's Defense Advanced Research Projects Agency (DARPA) Defense Sciences Office (DSO), the first phase of the Trauma Pod project is being developed by a consortium of 12 firms led by SRI International of Menlo Park, CA, a developer of telesurgery systems.
In March, SRI announced the signing of a $12 million, two-year contract to develop the first phase of the project and integrate its components. DARPA is also funding a second parallel track to develop a highly instrumented gurney that will be combined with the Trauma Pod project in a later phase.
At the Society for Medical Innovation and Technology (SMIT) meeting last month, Pablo Garcia, senior research engineer at SRI's artificial intelligence center, talked about the Trauma Pod and the work ahead.
"Current conflicts in Iraq and Afghanistan have proven that bringing surgical care to the battlefield is very beneficial in reducing casualties and long-term injuries," Garcia said. "This has already been done by forward surgical teams in the Navy and the Air Force, and it's a very successful strategy ... but you can reduce casualties further if you can actually get faster care."
Some injuries, such as those to major blood vessels, require intervention within minutes rather than hours if the patient is to survive or avoid major disability. The lack of rapid response for critical injuries represents a huge unmet need in the military, he said.
"Being able to deploy these surgical facilities in a way that's very streamlined means that making them very light and very small is essential," Garcia said. "The problem is that there's a real trade-off here because the closer you start getting surgical resources to the casualty, the more at risk you put those precious resources."
Putting it on the road
Phase I of the Trauma Pod program is aimed at developing robotic technology to perform a completely unmanned surgical procedure in a fixed facility. As principal investigator and systems integrator for the project, as well as a technology contributor, SRI is working with 11 other developers on phase I.
Other cooperating companies include General Dynamics Robotic Systems of Westminster, MD, which builds unmanned ground vehicle systems, and the University of Texas at Austin, a designer of software control systems for material disposal and space manipulators.
The University of Maryland in Baltimore, which built the Operating Room of the Future, is lending its telesurgery expertise to the project along with the University of Washington in Seattle, a developer of surgical robotics. In New York City, Robotic Surgical Tech has designed a "robotic nurse" named Penelope, later versions of which may find their way into the Trauma Pod project.
Phase II will focus on miniaturizing the various components for deployment in a mobile platform, Garcia said. This second phase faces myriad challenges, including the need for expanding surgical capabilities, and incorporating anesthesia, cleaning, and sterilization of instruments. Phase II will also see the merging of imaging results with the robotic manipulation. New technologies will be developed to enable faster bleeding control for critical cases.
"We'll be able to use not only mechanical instruments, we're also looking at using energy because energy doesn't require supply to follow along behind it, whether we use high-intensity focused ultrasound or some form of laser tissue welding," said Dr. Richard Satava, a professor of surgery at the University of Washington, who oversees all five of the ultrahigh-tech DARPA projects. Energy-directed instruments can be used to coagulate bleeding, as well as seal tissues together, he explained.
Finally, phase III will pull everything together with installation of the system in an unmanned vehicle for testing and eventual deployment. Additional subsystems will be developed for deployment in a mobile platform, and to enable the system to handle complex anomalies, according to Garcia. "We need a good box" to hold and transport the components, Garcia said.
Getting robots to cooperate
But for now the focus is on the initial phase, which will culminate in the performance of a medical surgery procedure without human intervention, according to Garcia. This phase includes automatic supply dispensing and tool changes, which are targeted to occur in 10 seconds, and demonstration of the whole-body CT scan, or more accurately a pseudo-CT scan, Garcia said.
The demonstration will place a shunt in an iliac vessel, Garcia said. "It typifies the kind of noncompressible injury that you have on the battlefield," and which affect the major vessels in the abdomen or extremities.
Phase I does not include the tricky task of coordinating the movements of the surgical robot with the robotic arm. Multiple robotic systems will eventually need to work around the patient together in a very tight surgical space without colliding or impeding each other's work.
"All the robots have to be choreographed and synchronized so that the final goal is accomplished," Garcia said. Every task performed and every tool and supply used are tracked and documented in real-time, and a medical history is generated based on this information during the procedure.
"Surgeons in the battlefield complain that surgical information is not passed on to the next session," Garcia said, but he said the problem would be eliminated by the automated record, since everything that happens passes through the central computer.
The medical encounter record generates an XML-formatted document containing the patient's medical history, triage information, preoperative diagnosis, surgical notes, and nursing documentation -- all generated automatically, he said.
Meanwhile back at the manned base, a human surgeon deploying a graphic user interface "needs to be able to conduct the surgical procedure as effectively as he would do it in the operating room, and this is not an easy thing to do," Garcia said.
Whole-body imaging
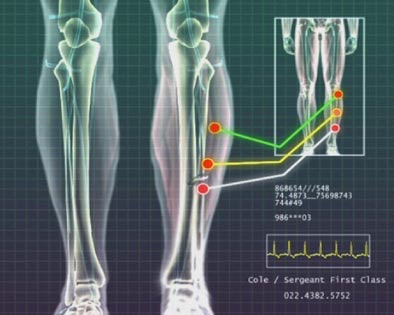
Ultimately, a small CT scanner is envisioned for automated full-body imaging and image reconstruction in the Trauma Pod. For phase I, however, imaging data will be acquired on a limited-angle tomographic x-ray scanner being developed by GE Global Research of Niskayuna, NY.
The prototype tomosynthesis unit generates images with resolution (pixel pitch) of 200 um. But like the other components in the Trauma Pod, it is not yet light enough or portable enough to be deployed in the mobile unit, according to Garcia.
The prototype consists of "an advanced flat-panel x-ray imager integrated into a stretcher and an x-ray tube in an open gantry arrangement above the patient," Joseph Manak from GE Research explained in an e-mail. "Using this system one acquires a large number of images of the patient at a variety of different angles by moving the x-ray source in a plane above the patient."
The images are then reconstructed into a three-dimensional volume with high resolution (equivalent to a flat-panel x-ray) in the plane parallel to the detector with somewhat less depth resolution. The resulting images are similar to coronal reformations from CT datasets, he stated.
Coronal slices allow the radiologist to quickly assess major areas of injury, and the system can obtain 3D diagnostic tomographic images rapidly for injury assessment, while supporting interventional procedures in 2D flouroscopic mode. So far the work has been preliminary.
"We've been doing some simulations and lab acquisitions to see how the system is working," Manak told AuntMinnie.com by telephone. "We've had some radiologists look at the images, and they've said these are pretty good images for trauma."
In order to install a CT scanner in a later phase of the Trauma Pod, as the project leaders want to do, the medical robots will have to be made small enough and flexible enough to work inside a CT bore.
"Until then you need a more open system like the one I am working on," Manak explained.
Supply side
Medical supplies and tools will be served up by a robotic arm from drawers in a toolbox and a supply box. At present these tools and supplies are all designed to be handled by humans, however, and so will need repackaging and in some cases redesign, Garcia said. Margins of error in movement and control of the components must be minimized to ensure that supplies are grasped correctly and the robots don't run into each other.
 |
 |
| Automated tool change and supply delivery demonstration, May 2006. Video courtesy of the U.S. Defense Advanced Research Projects Agency (DARPA) and Dr. Richard Satava. |
The Da Vinci robot (Intuitive Surgical, Sunnyvale, CA) was chosen as the official surgeon because of its already advanced capabilities, Garcia said. Like the scanner, the surgical robot is too large in its current form to operate in a mobile unit, and will need to be miniaturized.
An industrial manipulator and a rack system to dispense and store tools have also been selected, with the capacity for about 15 tools or different kinds of supplies. The fast cache, a sort of automated mail tray, will serve as a temporary holding area that provides fast access for tools and supplies that are needed quickly.
Storing bandages in the fast cache, for example, will shave valuable time from the task of resupplying each one from the toolbox, Garcia said. The fast-access storage tray will also cut down on the number of robot movements and computer instructions needed to drive and coordinate them.
Software is being developed to coordinate the enormous number of tasks that will need to be accomplished. Dispensing a simple supply requires as many as 150 separate steps, Garcia said.
The system comprises six major components including the Da Vinci surgical robot and the robotic arm, which are already installed in a mock operating theater.
The emulator is the brains of the system. Its processors are loaded with the software needed to control each component and make them work together. The console is a graphic user interface by which the human surgeon will communicate with the components.
The Trauma Pod is being designed from the start to be flexible and scalable, Garcia said. "This phase of the project is more about setting up the right infrastructure (for) future phases. As robots become more adequate for the objectives that we're trying to accomplish they can be just put into the system."
The system will be capable of performing complex procedures, Garcia promised. "Whatever Da Vinci can do now, we can do," he said.
The project aims to bring the latest surgical technology as far forward in the battlefield as possible. However, there are just as many potential nonbattlefield applications, DARPA project manager Satava wrote in an e-mail to AuntMinnie.com.
"The fundamental revolution in robotic surgery is not the robots, but rather that we now have a system which a surgeon can use that integrates all the separate parts of surgery (preoperative triage and care, surgical procedure, and postoperative maintenance of care) in a single integrated system," he stated. "This is the power of information-age technologies integration."
By Eric Barnes
AuntMinnie.com staff writer
June 26, 2006
Related Reading
Image guidance evolves into imaging therapy, May 12, 2005
ECR imagines radiology's future, March 3, 2005
NEMA paper touts imaging's role in oncology, April 6, 2006
CARS suite of the future sees key role for image-guided intervention, June 23, 2005
Copyright © 2006 AuntMinnie.com




















