When it comes to 2D versus 3D virtual colonoscopy, there's not a right or wrong choice for primary reading. The optimal visualization method might depend on the particular lesion, or the method the reader is accustomed to. And whichever method you use to find a lesion, you'll need the other to confirm it.
At Stanford University's International Symposium on Multidetector-Row CT in San Francisco, Dr. Judy Yee discussed the pros and cons of each primary reading method, and cited studies attesting to the superiority of one or the other. Yee is chief of radiology at the San Francisco Veterans Affairs Medical Center and professor and vice chair of radiology at the University of California, San Francisco.
Before 2003, 2D was considered the best way to look for polyps, and in any case few 3D options were available for primary interpretation. Then came Dr. Perry Pickhardt and colleagues' U.S. Department of Defense study, which used primary 3D reading on a Viatronix (Stony Brook, NY) workstation and was accurate enough to beat optical colonoscopy performed by experts (New England Journal of Medicine, December 4, 2003, Vol. 349:23, pp. 2191-2200).
Today "there really is no controversy -- you need to use both 2D and 3D," Yee said. "You can have a preferred method for using 2D predominantly and going to 3D for problem solving. Or you can use 3D predominantly and use 2D for problem solving."
To perform 2D primary viewing, scroll through the data until you find a lesion, then bookmark it, she said. At that point the workstation software should take you to the same spot on 3D where you confirm the lesion.
"You need a workstation that will allow you to bring up your supine and prone axial imager on the same display," she said. "You're going to view the images somewhere between a lung window and a lung and a bone window, and you're going to systematically and interactively scroll through each segment of the colon. I like to start distally in the rectum and work my way, centimeter by centimeter of colon, to the cecum."
In her abstract, Yee recommended a standardized high-contrast display window (width 1500, level -200) for primary 2D interpretation to maximize polyp visualization in the air-soft-tissue interface, and for displaying air or heterogeneous densities within residual stool. Use a standard soft-tissue window (width 400, level 10) to evaluate mural involvement of cancers, characterize the fat density of lipomas, and evaluate extracolonic structures, she said.
When you find a lesion you'll need to confirm it on 3D, Yee said. If you're not finding lesions you should be finding, maybe something else is wrong.
"I think the two biggest mistakes that are made when you're first reading primary 2D is that you don't magnify enough and you scroll too fast," she said.
As for 2D's advantages, "interpretation time has been shown to be shorter compared to primary 3D," Yee said, and there is wider availability of 2D axial and MPR displays. Two-dimensional viewing offers high sensitivity for polyp detection in adequately cleansed and distended colonic segments, and requires a minimum amount of processing and graphics hardware. And when fecal tagging is part of prep, 2D enables interpretation without subtraction software, which is still in development.
 |
With primary 2D, "you can see the density of the lesions, so automatically you can exclude stool if you see air in it, or fatty lesions," she said. "You can discount diverticula very easily on 2D."
Disadvantages of 2D include the difficulty of tracking the colon with redundant segments, aberrant anatomy, or multiple collapsed segments, Yee said.
 |
Pros and cons
Faster processors, better graphics cards, and software have significantly advanced 3D visualization and navigation in recent years, Yee noted. For a primary 3D read, the software must first segment the colon and draw a centerline. If fecal tagging is used, digital subtraction of fecal material must be implemented to maintain acceptable levels of accuracy.
"Remember you're going to have to do four fly-throughs -- you're flying antegrade and retrograde in both supine and prone (positions)" with 2D confirmation of abnormalities, she said. "Again you're going to bookmark your lesions and autotransfer to 2D to see if you have stool or a real soft-tissue lesion."
Primary reading with 3D can be a little smoother. "You can basically hit a key and sit back and watch for lesions," Yee said. And primary 3D is easier to learn for some, she added.
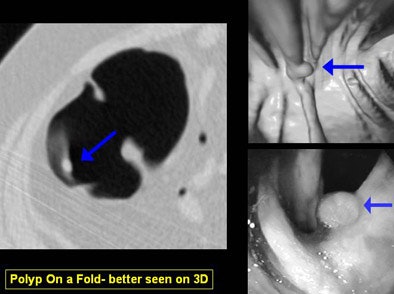
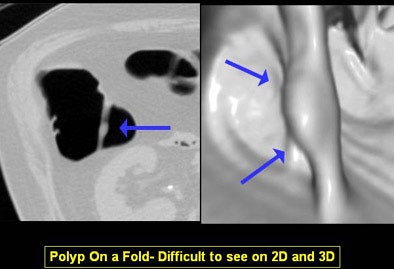
"You can differentiate folds from polyp and easily detect polyps on folds," she said. "And as shown in the Pickhardt study, you can achieve really high levels of sensitivity and specificity."
The primary 3D reader can also deviate from the flight path at any time to evaluate suspected lesions, and software can track which areas of the mucosa have been examined, Yee said. 3D can demonstrate complex, bulbous, or merging folds better than 2D.
The disadvantages include generally longer interpretation times with 3D, in addition to the time needed to process image data before it can be read. Some pitfalls are also unique to the 3D visualization process -- which can result in missed lesions or false-positive renderings of data, she said.
"Annular carcinomas are better evaluated on 2D views, and may be mistaken for an area of collapse on 3D," Yee wrote in her abstract.
 |
A third option is the dissection view, Yee said. This method splits the colon along its axis, offering views of very large areas of the colon at once. It may also be very easy to learn, she said, citing a study that demonstrated faster interpretation times but lower sensitivity compared to 3D endoluminal viewing.
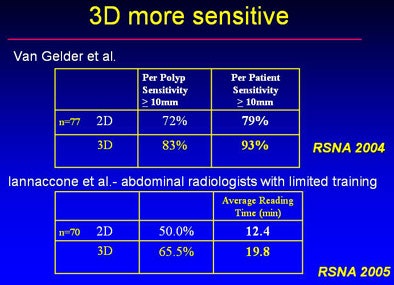
At a 2005 RSNA session on 2D versus 3D that Yee chaired, two studies showed that 3D had higher sensitivity than 2D. But two others showed equivalent sensitivity, and with shorter viewing times for 2D.
 |
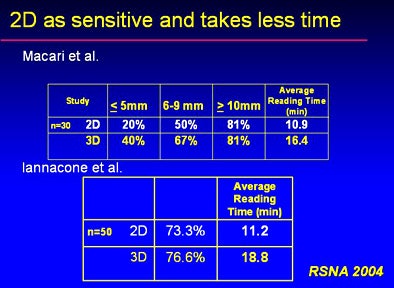 |
"We do know that primary 2D has shorter interpretation times compared to primary 3D," Yee said. "I think if you're well-trained, both methods can have high sensitivity and specificity.... I really do believe there is no one right way to read (VC), you really have to use both."
Other recent studies
A paper in the June Radiology assessed whether 3D viewing could improve radiologists' accuracy in classifying true- and false-positive polyp candidates identified by CAD (Radiology, June 2006, Vol. 239:3, pp. 768-776).
Dr. Rong Shi; Dr. Schraedley-Desmond, Ph.D.; Sandy Napel, Ph.D.; and colleagues from Stanford University Medical Center in California examined 47 VC datasets. Four experienced readers classified 705 polyp candidates (53 true-positive and 652 false-positive candidates) detected with CAD. Initial 2D viewing was followed immediately by combined 2D and 3D.
Compared to optical colonoscopy results, 3D viewing improved the classification of true- and false-positives for three readers, and increased the area under the ROC curve for each reader to 0.96-0.97 (p < 0.001).
"For (true-positive) candidates, maximum polyp width (p = 0.38), polyp height (p = 0.19), and preparation (p = 0.004) significantly affected accuracy," Shi and colleagues wrote. "For (false-positive) candidates, colonic segment (p = 0.007), attenuation (p < 0.001), surface smoothness (p <0. 001), distension (p = 0.034), preparation (p < 0.001), and true nature of candidate lesions (p < 0.001) significantly affected accuracy."
The group concluded that 3D viewing increased reader accuracy significantly in the classification of polyp candidates. Not surprisingly, polyp size and exam quality were also significantly associated with accuracy.
"As preliminary data, these observations suggest that 3D viewing remains important for maximizing performance of human readers, even when (VC) interpretation is augmented by CAD," they wrote.
On the other hand, 2D primary reading was the winner in another June study. The overall performance of the two methods was comparable, wrote the authors, including Dr. Stuart Taylor of St. Mark's Hospital and Dr. Steve Halligan from Charing Cross Hospital, both in London (Radiology, June 2006, Vol. 239:3, pp. 759-767).
However, 3D yielded lower sensitivity and more false positives compared to 2D, and took significantly longer to complete. The results showed that mean sensitivity values for polyps measuring 1-5 mm, 6-9 mm, and 10 mm or larger were 14%, 53%, and 83%, respectively, for 2D plus CAD reading, and 16%, 53%, and 67%, respectively, for primary 3D analysis.
By Eric Barnes
AuntMinnie.com staff writer
July 28, 2006
All images and charts courtesy of Dr. Judy Yee.
Related Reading
2D primary reading plus CAD has an edge in VC study, July 11, 2006
Reading method, insufflation affect polyp measurements, November 4, 2005
Polyp measurements more accurate in 3D, September 6, 2005
Debate over 2D versus 3D VC reveals subtle differences, January 21, 2005
Copyright © 2006 AuntMinnie.com