Multidetector-row CT (MDCT) and advanced 3D processing are a powerful combination when it comes to examining the small intestine and its surrounding structures.
Researchers from Korea discuss the limitations of techniques such as CT enterography when compared with noninvasive 3D imaging, and recommend exam and contrast protocols that can add value to images acquired at 16-detector CT, in this month's American Journal of Roentgenology.
"Small-bowel follow-through (SBFT) and enteroclysis are widely used for small-bowel imaging; however, these examinations provide only indirect information about the bowel wall and surrounding structures, and are prone to problems caused by overlapping bowel loops," wrote Drs. Seong Sook Hong, Ah Young Kim, Jae Ho Byun, and colleagues at the University of Ulsan College of Medicine in Seoul (AJR, November 2006, Vol. 187:5, pp. 1212-1221).
Although CT enteroclysis benefits from excellent bowel distension and the ability to assess extraluminal disease, it comes with the major drawbacks of invasiveness and high radiation exposure, they explained. And although wireless capsule endoscopy is another alternative, it has important limitations of its own.
"The value of (capsule endoscopy) is well-documented for diagnosing obscure gastrointestinal bleeding and early Crohn's disease," the team wrote. "However, problems with this technique include capsule obstruction by bowel strictures and battery failure in prolonged transit (battery life is approximately seven hours). The technique may provide false-negative results if there is rapid peristalsis at a lesion site, or if there is bowel angulation at a lesion that impairs the camera view."
The authors' exams were all performed on a 16-slice scanner (Somatom Sensation 16, Siemens Medical Solutions, Malvern, PA) using 16 x 0.75-mm collimation, 0.75-mm slice width, 120 kVp, 165 mAs, and volume pitch of 16. Images were reconstructed at 1-mm intervals using a B-30 soft-tissue algorithm. Before imaging, the team injected 150 mL of nonionic iopromide contrast media (Ultravist 370, Schering, Berlin).
Triphasic (unenhanced, arterial, and delayed-phase) CT was used to evaluate mesenteric ischemia and gastrointestinal bleeding without oral contrast.
The radiation dose was high, however. The CT dose index and dose-length product from a single dynamic-phase CT were high at 9.32 mGy and 526 mGy, respectively. So in patients with suspected small-bowel obstruction, inflammatory bowel disease, or neoplasm, a single or biphasic CT scan (delayed phase, unenhanced phase, or both) was acquired.
The oral water-soluble contrast agent meglumine diatrizoate (Gastrografin, Schering) is useful for opacifying bowel loops for diagnosing bowel obstruction, perforation, and gastrointestinal fistulization, the authors wrote. However, Gastrografin isn't appropriate in all cases because positive oral contrast can obscure opacified blood vessels or hinder the detection of bowel-wall changes such as bowel-wall enhancement.
"Although positive oral water-soluble contrast material did not interfere with 3D imaging in our patients, we preferred to use water as a neutral oral contrast material in patients with suspected ischemia," they wrote. "Neutral oral contrast material, such as water or methylcellulose, is recommended for the diagnosis of mesenteric ischemia or acute inflammatory bowel disease."
For mesentery ischemia, CT's critical role is to detect ischemic changes in the affected bowel loops and mesentery, and determine the cause of the ischemia, the authors wrote. Bowel distension, wall thickening, mesenteric edema, and ascites are helpful but nonspecific CT findings. Findings that suggest acute mesenteric ischemia can be readily seen at CT including splanchnic vascular occlusion, intramural gas, lack of bowel-wall enhancement, and multiorgan infarction, the authors wrote.
 |
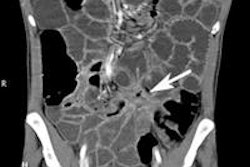
| In a 56-year-old man with acute mesenteric ischemia, neither emboli nor thrombi are definitively shown on axial arterial-phase CT (above). However, oblique coronal plane of volume-rendered image (below) shows large embolus (thick arrow) and extensive vascular occlusion (arrowheads) along the superior mesenteric artery and its branches, with multifocal renal infarction (thin arrows). Because this patient suffered from long-standing severe heart failure, mesenteric ischemia was conservatively managed with anticoagulant drugs. Images republished with permission of the American Roentgen Ray Society from AJR; 2006; 187: 1212-1221. |
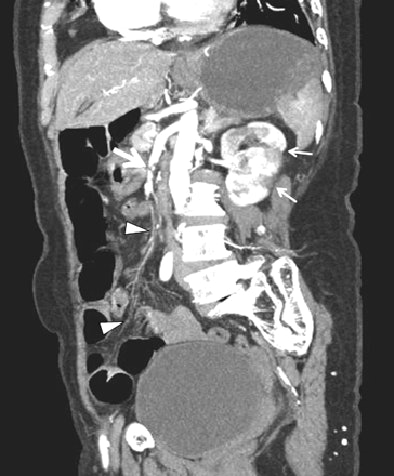 |
MDCT also shows mesenteric emboli and focal infarction of the bowel loops; most emboli wedge at branch points in the mid to distal superior mesenteric artery, usually distal to the middle colic artery. "Meanwhile, thrombosis is most likely to occur at or near the origins of the proximal mesenteric arteries," Hong and colleagues wrote.
Mesenteric venous thrombosis is an uncommon but potentially lethal cause of bowel ischemia. Predisposing factors include involvement of the superior mesenteric vein in 95% of cases, while chronic mesenteric ischemia is primarily caused by atherosclerosis of mesenteric arteries, which can be readily seen at CT.
Nonocclusive mesenteric ischemia is a common cause of acute mesenteric ischemia, particularly among patients over 50 with cardiac dysfunction, the authors added.
Diagnosing mesenteric ischemia with CT does have drawbacks, however. For example, inadequate or nonopacified blood in the mesenteric vessels can lead to false positives, they wrote. Second, calcified atherosclerotic plaques in the mesenteric vessels are commonly seen in patients without clinical symptoms, while the small intestine often appears normal in patients with chronic mesentery ischemia.
"Therefore, clinical correlation with the CT findings is essential in the evaluation of patients with suspected mesenteric ischemia," the authors wrote.
Small-bowel obstruction can have serious sequelae if misdiagnosed or diagnosis is delayed, resulting in lethal or life-threatening complications such as ischemia and perforation. Imaging's role is to identify the presence of obstruction and the site, determine its severity and cause, and look for signs of strangulation, they noted.
Diagnosis depends on identifying a transition zone with dilated proximal bowel loops. However, overlapping dilated bowel loops often prevent depiction of a definite transition zone using only axial images, the authors wrote.
"In these situations ... 3D imaging can be helpful in evaluating indeterminate cases on the axial plane, such as volvulus or internal hernia," they explained. "The additional use of positive oral contrast can help to distinguish complete from incomplete bowel obstruction."
With strangulation obstruction, CT can show thickening and increased attenuation of the bowel wall; "serrated beak-like narrowing at the site of obstruction, target or halo sign, pneumatosis intestinalis, and gas in the portal veins have been reported to be suggestive of strangulation," the group wrote. Additional findings of haziness and hemorrhage can be seen in the mesentery attached to ischemic bowel loops.
"Advanced 3D image processing, such as slab volume rendering using MDCT, is more flexible than 2D multiplanar reconstruction, and also makes it possible to display unlimited planes with markedly reduced artifacts," they wrote.
In diagnosing inflammatory bowel disease, small-bowel series and enteroclysis do not provide critical information about the extraluminal extension of disease or changes in surrounding structures. However, CT is also limited in its ability to depict subtle mucosal changes or locate potentially fistulous tracts or bowel perforation.
3D imaging can be helpful in evaluating bowel inflammation complicated by fistulas or abscesses seen in Crohn's disease or tuberculosis.
"Three-dimensional volume rendering of MDCT performed with positive oral contrast can improve the visualization of the presence and site of both the structure and the fistula," the team wrote. "This valuable information from 3D CT may significantly improve the observer's confidence in interpreting the imaging and the clinician's or surgeon's understanding of the extent of disease."
Neoplasms of the small bowel are rare, and frequently overlooked due to their vague or nonspecific clinical manifestations. CT's most important role has been in preoperative staging rather than diagnosis, but MDCT is putting more emphasis on diagnosis, according to the authors.
CT's ability to demonstrate a tumor's vascular supply is a key strength of the modality, and for this reason a negative contrast agent such as water may be best because it will not obscure the opacified vessels, the group wrote. Yet water-soluble positive oral contrast is preferable when communication is suspected between the necrotic tumor and adjacent bowel, fistula formation, or perforation.
For determining the cause of obscure gastrointestinal bleeding, CT is still not comparable in sensitivity to scintigraphy or conventional angiography, but may be a viable alternative when more invasive procedures fail to determine the source of active bleeding, the authors wrote.
"MDCT and refined 3D imaging processes can offer a full examination of the small intestine and powerful information about the bowel and its surrounding structures," they wrote. "In most cases of small-bowel disease, various 3D techniques can help radiologists make an easy, rapid, and accurate diagnosis while avoiding unnecessary examinations."
Knowing how to use these CT techniques is essential to achieving the diagnostic goal of one-step imaging of the small bowel, they concluded.
By Eric Barnes
AuntMinnie.com staff writer
November 15, 2006
Related Reading
CT enterography can determine Crohn's disease severity, November 7, 2006
Capsule endoscopy helpful in identifying, managing small bowel tumors, November 2, 2006
Capsule endoscopy may miss postop recurrence of Crohn's disease, July 10, 2006
CT, CE are better choices for small-bowel Crohn's, January 25, 2006
Success begets growing role for CT enteroclysis, November 18, 2004
Copyright © 2006 AuntMinnie.com