
The noncontrast CT coronary artery calcium scoring scan does not detect all coronary artery disease, but it does have one big advantage over contrast-enhanced coronary CT angiography (CTA), the new cardiac imaging test on the block.
The advantage is calcium scoring's solid prognostic value in asymptomatic patients. Dozens of studies have demonstrated a robust association between high calcium scores and the risk of future adverse coronary events -- at least among asymptomatic individuals who happen to wander into a screening center and get scanned.
In individuals without detectable calcium, current guidelines estimate the annual risk of adverse events at about two per 1,000. The risk rises more than tenfold for those with calcium scores above 400 -- to about 20-50 events per 1,000 individuals -- each of whom has about a 15% chance of having obstructive coronary artery disease.
Yet the prognostic value of calcium scoring in individuals with chest pain or other symptoms suggestive of coronary artery disease -- i.e., those most in need of evaluation -- has not been proved.
Is there a prognostic benefit for coronary CTA, a promising exam that goes calcium scoring one better by opacifying the arteries with contrast before imaging? None that has been demonstrated so far. Certainly CTA does a good job of identifying clinically significant stenoses, yielding greater than 90% sensitivity in most studies. Research suggests a real patient benefit in CTA's ability to identify the "culprit" stenotic lesions that are likely to cause future events, particularly among patients at moderate risk of having coronary artery disease.
Years of large randomized multicenter trial results and patient follow-up will be needed to determine whether CTA has a prognostic value, or can potentially reduce morbidity and mortality in these patients by altering their management.
At least one group has a head start on the question. In an effort to prospectively evaluate the prognostic value of coronary CTA, researchers at the Weill Cornell College of Medicine in New York City performed a study of 1,127 patients over age 45 (mean age 59) presenting with chest pain or other symptoms suggestive of coronary artery disease. All were examined with 64-detector-row CT angiography.
The results showed that the extent and severity of coronary artery disease at CTA correlated strongly with death from all causes.
Dr. James Min, director of cardiac CT and assistant professor of medicine and radiology at Weill, discussed the study results on Saturday at the International Symposium for Multidetector-Row CT sponsored by Stanford University, and with AuntMinnie.com in an interview.
Prognostic power is essential for any test, particularly for the management of symptomatic heart patients who come into the office caring less about statistical risk and more about "whether they're going to live or die," Min said.
Coronary CTA hasn't shown an ability to predict outcomes yet, and while nuclear medicine does have a strong prognostic value -- "that's its claim to fame," Min said -- the results aren't specific to the affected coronary vessels. And the results are questionable if SPECT and CTA are discordant.
"What do you do when the SPECT is good but the CTA is bad?" he said. "Which one wins -- anatomy or physiology?"
In the study, Weill researchers graded each stenosis found at 64-slice coronary CTA as minimal (< 30%), mild (30% to 49%) or severe (≥ 70%). A modified Duke coronary artery jeopardy score (originally designed for invasive coronary angiography) was also used to evaluate plaque in the right coronary artery, left anterior descending artery, left circumflex artery, and left main artery.
"We followed the patients for 15 months, and we looked at overall coronary plaque burden in the three major epicardial vessels by several different methods," Min said. During follow-up, death from all causes was examined using Cox proportional hazards models adjusted for the pretest likelihood of coronary artery disease. The Social Security Death Index was used to verify mortality.
Stenoses detected at CTA were strongly associated with all-cause mortality, Min said.
MDCT predictors of death included the number of vessels with moderate (≥ 50%) or severe (≥ 70%) stenosis, along with proximal left anterior descending artery stenosis (p < 0.001 for all).
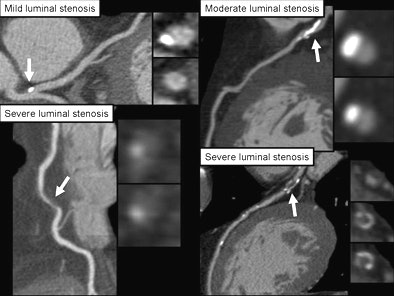 |
| Each stenosis detected at coronary CTA was graded as minimal (< 30%), mild (30% to 49%), or severe (≥ 70%). All images courtesy of Dr. James Min. |
According to the results, "if you have more severe plaque in one, two, or three vessels, or in the left main artery, you tend to die more," he said. "There is a stepwise reduction in survival depending on how many vessels have severe plaque."
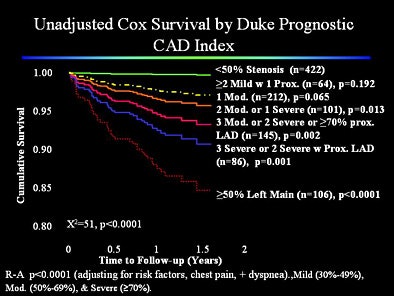 |
Patients with mild or no coronary artery plaque had a very high survival rate (99.7%), while those with at least moderate left main artery stenosis had lower survival rates (85%, p < 0.001).
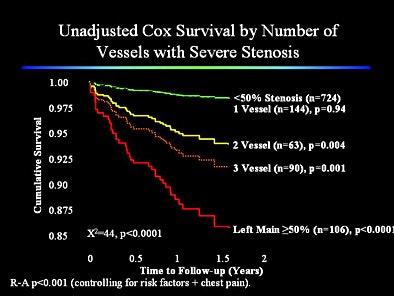 |
"CTA really is a good predictor of all-cause mortality," Min said. Of equal import, normal or mildly abnormal measures of coronary artery plaque at CTA conferred a high survival rate. The negative predictive value for death was 99.7%.
"If you don't have disease at CTA you don't die, and that's a great thing to be able to tell your patients," he said.
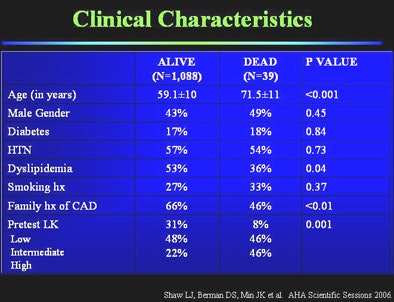 |
The research was limited by the lack of a randomized double-blinded design and other algorithms that serve as traditional measures of disease risk, Min said. Perhaps more important, it was limited to a single facility. And CTA results might be less useful in facilities where CTA was poorly performed.
The study is ongoing, and the next update will include not only all-cause mortality, but cardiac and noncardiac causes of death in about 2,000 patients. A review of the data confirmed that none of the deaths during the follow-up period could be attributed to the CTA itself, or from any intervention ordered as a result of it, he added.
As for noncontrast CT coronary artery calcium scoring, it is simply a different test for a different group of patients, according to Min. "We don't have any evidence that it's useful in a symptomatic cohort," he said. "If we're going to talk about it and keep doing it, then we should prove it. And we don't have that data." Nuclear medicine studies are prognostic, but inadequate to guide early stenotic disease intervention.
SPECT is "a great test," but is limited because it is based on relative perfusion, Min said. Theoretically, if several coronary arteries were equally stenosed, whether at 50% or 80%, the SPECT results would still be normal. "It only works if one vessel is much worse than the other vessels," he said.
"I think the paradigm needs to shift, and that we need to shift that paradigm to change imaging for intervention -- which is what we do with nuclear, where we identify severe disease -- to imaging for prevention, where we identify coronary artery disease much earlier, and utilize favorable lifestyle modifications and medicines to try to present those first myocardial infarctions from ever occurring," Min said. And a test should not only be able to identify patients at risk, but "exclude those patients who aren't at risk, so the next time they come in for chest pain we don't have to start the workup all over again."
By Eric Barnes
AuntMinnie.com staff writer
June 19, 2007
Related Reading
Inverse-geometry CT project promises higher image quality, fewer artifacts, June 14, 2007
Image postprocessing boosts performance of multidetector CT coronary angiography, May 31, 2007
Study correlates CTA to angiography, myocardial perfusion SPECT, May 25, 2007
Dual-source coronary CTA images the calcium-burdened, April 13, 2007
Copyright © 2007 AuntMinnie.com




















