A British study of symptomatic patients undergoing same-day virtual and conventional colonoscopy found the two methods equivalent for the detection of clinically significant polyps. In fact, the segmentally unblinded results showed that virtual colonoscopy (VC or CT colonography [CTC]) did slightly better than optical colonoscopy (OC) for the detection of clinically significant polyps 6 mm and larger.
"Further studies are required to validate the potential value of VC as a primary colonic imaging modality," wrote study authors Dr. Owen Epstein, Dr. James Bell, and colleagues from the Institute for Minimally Invasive Gastroenterology, Royal Free Hampstead NHS Trust in London.
"This study is the first to compare virtual colonoscopy software (Viatronix V3D Colon, Stony Brook, NY, version 1.2) with OC in symptomatic gastroenterology outpatients, and uses this information to assess the potential impact of VC on diagnostic and therapeutic OC" (Alimentary Pharmacology and Therapeutics, September 1, 2007, Vol. 26:5, pp. 727-736).
The study examined 100 patients age 50 and older with same-day virtual and optical colonoscopy. All had been referred for indications of a higher risk for polyps and colon cancer, such as a change in bowel habits (n = 28), abdominal pain (n = 21), microcystic anemia (n = 16), weight loss (n = 13), or a family history of colon cancer (n = 11).
The patients followed a low-residue diet for three days prior to the procedure. On the last day before imaging they consumed only clear fluids and a laxative single packet of Picolax (sodium picosulphate and magnesium citrate, Ferring Pharmaceuticals, Langley, U.K.) along with 10 mg of bisacodyl. Stool tagging was achieved with a 2% barium solution (E-Z-CAT, E-Z-EM, Lake Success, NY). Before imaging, 50 mL of Gastrografin (Bayer Schering Pharma, Berlin) was administered.
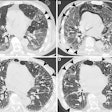
Following manual insufflation of the colon with room air, prone and supine CT images of the abdomen were acquired on a four-slice LightSpeed scanner (GE Healthcare, Chalfont St. Giles, U.K.). Images were acquired at 1.25-mm collimation, 50 mAs, and 120 kVp, and the total effective radiation dose for the combined prone and supine studies was 5.8 mSv.
Patients underwent optical colonoscopy after VC was completed. OC was performed by experienced gastroenterologists who had previously achieved cecal intubation rates of 90% or greater, Bose et al explained.
The CT data were examined using the Viatronix primary 3D bidirectional fly-through software, with 2D used for problem solving. Extracolonic findings were documented in a separate search and graded for clinical importance. All detected polyps were recorded by segment and location, and uncertain findings that had been labeled as a possible polyp or as fecal material were deemed false positives if they were not found at OC, the authors explained.
"For a reported lesion to be recorded as a true positive, the lesion had to appear in the same segment or in adjacent segments, and the two recorded diameters had to be similar (within a 50% margin of error)" the group reported. Results showed a good correlation between VC and colonoscopist-reported polyp size (rs 0.7, p < 0.02).
VC was successful in all but one (99/100) patient who was unable to retain the room air colonic insufflation; it was abandoned in another patient who experienced "profound bradycardia," according to the authors.
Optical colonoscopy was successful in 91 patients. The causes of OC failure in the other nine patients included uncontrolled bowel looping, severe sigmoid diverticulosis, or pain.
OC found 69 diminutive polyps, five of which were detected on segmental unblinding of VC results. Histology, available in 60 diminutive polyps, included 25 (42%) benign tubular carcinomas and 35 (58%) nonadenomas. Diverticulosis was diagnosed at CTC and optical colonoscopy in 36 and 20 patients, respectively, and diverticulosis was reported in 16 patients only at CTC, the team noted.
In 90 of the 100 patients who underwent both procedures successfully, both VC and OC showed the three cancers detected. Optical colonoscopy revealed 10 polyps ≥ 6 mm for a sensitivity of 91%, while VC found 11 confirmed polyps of the same size (sensitivity 100%). After segmental unblinding of VC results, an additional 15-mm polyp was confirmed at colonoscopy.
All patients reported that they were able to tolerate the bowel prep, and there was no reported overall preference among patients for either VC (mean pain score, ± SD, 4.39 ± 2.2) and OC (mean pain score ± SD 4.56 ± 2.08). Automated insufflation with CO2, which was not available at the time of the study but is now in routine use, might have reduced the discomfort further in virtual colonoscopy, the group wrote.
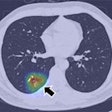
In all, VC revealed 175 extracolonic findings in 72 patients, 22 of which were deemed high in significance and 34 of medium significance. "This collateral information might add to the clinical assessment of patients presenting with abdominal symptoms where colonoscopy fails to reveal a likely cause," Bose and colleagues wrote.
As previously reported by Pickhardt et al and other researchers, 3D primary visualization provides a longer time frame than 2D for the detection of clinically important polyps, the study team wrote. And the software's "paint" feature color-codes the area of mucosa visualized during VC interpretation, in this study indicating 99% of the mucosa was covered on average.
In symptomatic patients, primary 3D VC is "equivalent to optical colonoscopy for diagnosing colon cancer and clinically significant polyps," the group wrote, adding that a case could be made for the use of 3D VC followed if necessary by same-day OC.
"In our view, the era has arrived where patients can be judiciously be offered VC as a credible alternative to diagnostic OC," they concluded. "In addition to offering a primary screening modality, VC should be considered in symptomatic adults where the clinician wishes to exclude polyps, cancer, strictures, and diverticulosis as a cause of symptoms, or where OC has failed to reach the cecum."
By Eric BarnesAuntMinnie.com staff writer
September 12, 2007
Related Reading
Significant extracolonic cancer found in VC screening patients, June 12, 2007
'Filet view' VC software pares reading time, August 28, 2007
Screening model calls VC most cost-effective colon exam, April 24, 2007
Higher costs seen in post-VC extracolonic follow-up, November 3, 2006
Group credits 3D reading for best-ever VC results, October 15, 2003
Copyright © 2007 AuntMinnie.com