
Neither the primary reading method (2D versus 3D) nor reconstruction slice thickness affected VC results in significant ways in a recent study by researchers from the Mayo Clinic in Rochester, MN.
The results in a midsized cohort of 452 asymptomatic screening subjects who underwent both virtual colonoscopy (VC or CT colonography [CTC]) and conventional colonoscopy on the same day, also found that the novel "virtual dissection" viewing method saved reading time, in accordance with previous reports.
"Controversy remains about the best image display for accurate interpretation and the optimal CT technique for scanning," wrote Drs. C. Daniel Johnson, Joel Fletcher, Robert MacCarty, and colleagues in September's American Journal of Roentgenology. "New techniques such as the 360º virtual dissection present the 3D endoluminal data as if the colon has been straightened and unfolded, allowing quick inspection of its mucosal surface" (AJR, September 2007, Vol. 189:3, pp. 672-680).
An advantage of virtual dissection is elimination of the need for the bidirectional fly-through in 3D, forward and backward, through CT image data, which can add reading time to 3D endoluminal viewing, the authors explained. On the down side, virtual dissection produces a midline trace and architectural distortion, which can hamper reading.
The three-year study (2001-2004) was designed before fecal and fluid tagging, drier bowel preparations, and automated CO2 insufflation were in common use for virtual colonoscopy, and as a result the number of noninterpretable segments was higher than expected, the authors stated, adding that the core aims of the study -- comparison of different reading methods and reconstruction slice thicknesses -- remain valid.
Among the researchers' take-home points: There is a trade-off between slice thickness and noise that radiologists should consider when acquiring CT data for virtual colonoscopy. Newer multidetector-row CT scanners can easily acquire submillimeter sections, but if radiation dose is left unchanged during thin-section acquisition, image noise increases, potentially introducing image artifacts that can increase the incidence of false positives.
The study aimed to compare the performance of primary 3D reading using virtual dissection with 2D primary reading, as well as 2.5-mm versus 1.25-mm scanner collimation.
The 452 asymptomatic subjects (56% men, 44% women) underwent both virtual and conventional colonoscopy after undergoing a cathartic prep (polyethylene glycol [82% of patients] or magnesium citrate [300 mL] plus bisacodyl tablets [3%] or 90 mL oral saline [15% of patients]), as determined by the referring physician. Ninety-two percent also received glucagon hydrochloride as an antispasmodic prior to manual insufflation of approximately 2 L of CO2.
Scanning was performed on an 8-detector-row system (LightSpeed Ultra, GE Healthcare, Chalfont St. Giles, U.K.) using 1.25-mm collimation, 1.25-mm and 2.5-mm reconstruction intervals, 70 mAs, and 120 kVp.
Three radiologists experienced in VC interpretation read the images on a GE Advantage Windows workstation using Voxtool 5.4.46 CT colonography software (GE Healthcare), a method that can display multiplanar 2D and 3D images. Whenever radiologists examined the same data twice using different viewing method, the reading was separated by at least six weeks' time to minimize recall bias, Johnson and his team wrote.
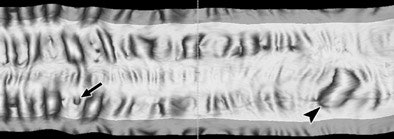 |
| Correlation of 3D endoluminal virtual dissection display with traditional images at CT colonography in the sigmoid colon of a 70-year-old man (above). Typical 3D endoluminal virtual dissection display of a 15-cm colonic segment. Diverticulum (arrow) and prominent fold (arrowhead) are correlated with 2D multiplanar and perspective, volume-rendered images for diagnosis. Below, 2D transverse image shows diverticulum (arrow) also seen above. Images republished with permission of the American Roentgen Ray Society © from AJR 2007; 189: 672-680 by C. Daniel Johnson, Joel G. Fletcher, Robert L. MacCarty, Jay N. Mandrekar, William S. Harmsen, Paul J. Limburg, and Lynn A. Wilson. |
 |
Following VC, standard index colonoscopies of each patient by experienced gastroenterologists were performed and videotaped during withdrawal of the colonoscope.
In all, the researchers found a total of 64 adenomas 6 mm or larger, including 26 large adenomas 1 cm or larger in diameter. Lesions smaller than 6 mm were not analyzed.
To evaluate radiologists' judgment of lesion presence (from "doubtful" to "highly confident") among the various reading methods, ROC curves were generated and the area under the curve (AUC) calculated for each of the three reviewers. The analysis found no significant difference in radiologists' performance between 2D and 3D detection or between 1.25-mm and 2.5-mm reconstructions (p > 0.05 for both).
"For adenomas 6-9 mm in diameter, the area under the receiver operating characteristic curve (AUC) using 2.5-mm datasets was 0.66, 0.62, 0.90, and 0.78, 0.69, 0.67 for reviewers 1, 2, 3, respectively, using primary 3D versus 2D search (p = not significant)," they wrote. "For neoplasms ≥ 10 mm, the AUC using the 2.5-mm datasets was 0.74, 0.85, 0.89 and 0.66, 0.86, 0.92 for reviewers using 2.5-mm primary 3D versus 2D search (p = not significant)."
Double reading improved lesion sensitivity in 84% (16/19) and 95% (18/19) for detecting large neoplasms using 2.5-mm and 1.25-mm collimation, respectively (p = not significant). Double reading was less effective for polyps 6-9 mm, yielding slice thicknesses of 2.5% and 1.25%, respectively.
Whereas the 2D search found four of five primary adenocarcinomas, 3D detected all five of five, they noted. Colonoscopy initially found 20 of 26 (77%) large lesions. Missed at colonoscopy but found at VC and later confirmed were four adenocarcinomas, one tubulovillous adenoma, and one tubular adenoma, Johnson and colleagues reported.
Residual fluid was rated mild (53%), moderate (34%), or nondiagnostic (3%) in 90% of patients. Residual stool was deemed mild (40%), moderate (18%), or nondiagnostic (3%) in 61% of all patients. Colon distension was rated adequate in 30%, suboptimal in one segment in 55%, and suboptimal for more than one segment in 55%, the team noted. The rate of nondiagnostic scans (13%) was "higher than expected," and probably attributable to the use of manual CO2 insufflation, a study limitation, and moderate or severe residual fluid in 26% of scans may have also reduced reading accuracy, the authors wrote.
Another limitation was the lack of stool tagging when the study was initiated in 2001, though specificity was high even without stool tagging. "The study remains relevant because the techniques were performed similarly," the team wrote.
Average interpretation times for primary 2D and primary 3D were 14.5 minutes (range 2-56 minutes, SD = 6.2 minutes) and 10.4 minutes, (range = 1.5-27.2 minutes, SD 6 minutes), respectively. The 3D virtual dissection images were interpreted approximately 25% faster than 2D.
For detecting adenomatous lesions 6 mm or larger at VC, there was no performance advantage between reconstruction of 2.5-mm and 1.25-mm slice thicknesses or between 2D and 3D, the group concluded.
"Decisions regarding slice thickness should include consideration of patient dose, image noise, and radiologist preference," they wrote. "Combining primary 2D and primary 3D (dual interpretation) helps reduce interobserver variability and can result in accuracy rates comparable to colonoscopy."
By Eric Barnes
AuntMinnie.com staff writer
September 20, 2007
Related Reading
VC measurements more accurate than optical colonoscopy, May 30, 2007
2D, 3D primary VC have their own advantages, July 8, 2006
Window levels matter when viewing submerged polyps in VC, July 24, 2006
Reading method, insufflation affect polyp measurements, November 14, 2006
Polyp measurements more accurate in 3D, September 6, 2005
Copyright © 2007 AuntMinnie.com




















