A new study from the Netherlands found that manual polyp measurements in virtual colonoscopy (VC or CT colonography [CTC]) were a bit more accurate than an automated process based on polyp protrusion measurements. The automated scheme still came out ahead, however, because it eliminated interobserver variability.
Accurate polyp size measurement in virtual colonoscopy is key to appropriate management, wrote Cees van Wijk, Dr. Jasper Florie, and colleagues from Delft University of Technology in Delft and the Academic Medical Center in Amsterdam.
"The size of a detected polyp is of primary importance for diagnosis and decision making because size is related to the risk of malignancy," they noted. "Accordingly, it has been proposed that polyps with a diameter smaller than 6 mm require no further action, whereas polyps 10 mm or larger should be removed with colonoscopy. There is debate over the need for polypectomy for 6- to 9-mm polyps. Surveillance for growth with CT colonography has been suggested as a safe alternative. A reliable measurement technique is needed in this scenario," they wrote (American Journal of Roentgenology, May 2008, Vol. 190:5, pp. 1279-1285).
Previous studies of polyp measurements have produced uneven and occasionally conflicting results. A 2005 study in a human colon specimen found that 2D measurements were more accurate when colonic distension was suboptimal, while 3D measurement was more accurate in well-distended colons. Burling et al reported in 2005 that automated measurement, which required observers to choose a starting point for segmentation and size measurement, demonstrated better interobserver and intraobserver agreement than manual 2D measurement of spherical phantom objects. But the team later reported that 3D measurements had the "largest systemic error" in a human study that used conventional colonoscopy as a reference standard (Clinical Radiology, May 2007, Vol. 62:5, pp.145-151).
Pickhardt et al found manual 3D measurements to be significantly more accurate than manual 2D measurements, and attributed 2D measurement underestimation to suboptimal alignment of orthogonal multiplanar reformations in relation to the polyp axis.
"Several factors may explain the conflicting results: the types of objects used (phantom objects versus patient data), noise characteristics and scanner resolution, reader variation (interobserver and intraobserver), and reliability of the reference standard (colonoscopy) in patient studies," the team wrote. "We studied the accuracy and measurement variability of an automated measurement technique under varying scanning conditions and using both phantom data and patient data."
Their automated scheme was compared to both 2D and 3D manual measurements. Phantom data measurements were performed for two slice thicknesses and two orientations of the phantom data in the CT scanner.
"We hypothesized that the variability of automated measurement would be greater than the intraobserver and interobserver variability of human readers," van Wijk and colleagues wrote. The study included 23 phantom objects in the form of artificial polyps inserted in an acrylic resin cylinder.
Data were also acquired from scans of 10 patients (six men, four women; mean age, 59 years; range, 30-74 years) participating in a VC study that included patients at increased risk of colorectal cancer. They had a total of 11 colonoscopy-confirmed polyps: six polyps 10 mm or larger in eight patients, and five polyps 10 mm in diameter or larger in five patients. VC was followed by conventional colonoscopy in all cases.
Images of the phantom and the patients were acquired on a 64-slice MDCT scanner (Brilliance, Philips Healthcare, Andover, MA) at 100 mAs; 120 kV; 0.625-mm collimation. The phantom was scanned both parallel and at a 45° angle with respect to the scanner axis to obtain an oblique orientation of the main polyp axes with respect to the scanning direction.
"The phantom in parallel orientation was scanned once with a slice thickness of 3.0 mm; the slice thickness was 0.9 mm for all other scans," the researchers wrote. Measurement with sliding calipers served as the reference for the phantom data; the mean of two independent colonoscopic measurements was the reference for the polyps.
The automated measurement was developed for a computer-aided detection scheme, and was performed on an experimental version of a commercial workstation (ViewForum 6.1, Philips). The researchers compared automated measurement with manual 2D and 3D measurements by two experienced observers.
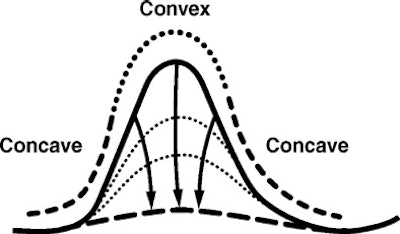
"The scheme entails estimation of the deformation of the colonic wall needed to digitally remove a presumed lesion," they explained. "For example, iteratively moving the points on the convex parts of the polyp (i.e., the protruding part) inward effectively flattens the object. After a certain amount of deformation, the surface flattening is such that the protrusion is removed. Thus the surface looks as if the object were never there. The amount of displacement is a measure of protrusion. The polyp is delimited by a threshold of the deformation field."
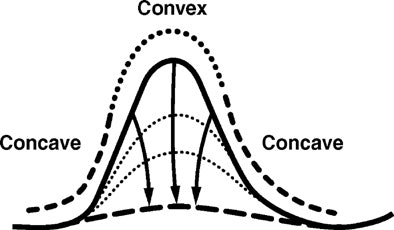 |
| Diagram shows cross-section of idealized polyp with deformed surface for estimation of protrusion. Republished by permission of the American Roentgen Ray Society, from "Protrusion Method for Automated Estimation of Polyp Size on CT Colonography," by C. van Wijk, J. Florie, C. Y. Nio, E. Dekker, A. H. de Vries, H. W. Venema, L. J. van Vliet, J. Stoker, and F. M. Vos, AJR 2008; 190:1279-1285. |
Automated polyp size was obtained by fitting an ellipse, and the polyp measurement was derived from the largest diameter of the ellipse, they wrote. Manual measurements in both 2D and 3D were performed by two experienced observers, who were asked to maneuver orthogonally over objects to measure their maximum diameter.
A Student's t-test was applied to assess systematic mean difference between paired measurements, and the standard variation of the mean difference was calculated to demonstrate measurement variability. Finally, a Bartlett's test was applied to test the assumption that standard deviations across measurement series were equal.
For phantom data, the measurement variability of the automated method was significantly less than that of the observers (p < 0.05) "except for the 3D measurement by observer 1, as follows: automated, 0.86 mm; observer 1, 1.76 mm (2D), 0.96 (3D); observer 2, 1.34 mm (2D), 1.45 mm (3D)," the group reported.
In patient data, the variability of the automated method did not differ significantly from that of manual methods. However, the automated method had a systematic error for phantom data (1.9 mm) that increased with polyp size. One of the observers also made a systematic error, undersizing polyps in both 2D and 3D measurements, likely due to the observer's different perception of the polyp boundaries.
Still, "Systematic error can be corrected with proper calibration," the group wrote. "This principle holds for measurements by observers and with an automated approach."
As for slice thickness, statistically significant differences in mean polyp size were found only between 3D measurements by both observers (p < 0.01). Here the variability of automated measurement was not significantly different from that of the observer measurements.
For phantom data, measurement variability in the automated method varied less than that of the observers "when either the orientation of a phantom (significant for 2D, not significant for 3D measurement) or slice thickness (significant for 3D, not significant for 2D measurement) was varied," van Wijk and colleagues wrote, suggesting that the finding may show that the reader variation of the automated method is less sensitive to data variation.
The automated approach also showed less variation than did the observers compared to the reference standard (significant for one of the two observers).
"This difference may be explained by the intraobserver variation, which was nonexistent for the automated method by definition," they added.
The study method is simpler than automated techniques that rely on region-growing schemes, and requires only that users indicate a specific protrusion, the researchers wrote. As a result, repeated measurements yield identical results regardless of seed placement.
There are limitations of the validity of comparisons owing to the use of different measurement techniques in different automated schemes, they wrote. In addition, the number of shapes used in the phantom was limited, and the patient cohort was small. The phantom was slightly denser than true polyps, and colonoscopy measurements were imprecise in their own right, the authors wrote.
"Our findings indicate that there is reduced variability in polyp size with automated measurement of phantoms," they concluded. "The variability of automated measurement is in the same range as that of manual measurement of polyps from patients. A clear advantage of the automated method is that it does not suffer from intraobserver variation. Moreover, the automated method can be calibrated once, whereas each observer may need individual calibration. Therefore, automated size measurement may well contribute to a practical evaluation strategy."
By Eric Barnes
AuntMinnie.com staff writer
May 21, 2008
Related Reading
Accuracy of polyp measurements depends on CT values, February 21, 2008
Colon polyps accurately measured using automated and manual 3D techniques, January 5, 2007
Reading method, insufflation affect polyp measurements, November 4, 2005
Polyp measurements more accurate in 3D, September 6, 2005
Copyright © 2008 AuntMinnie.com