Dynamic contrast-enhanced MR colonography (MRC) can readily distinguish benign from malignant strictures of the colon, according to Danish researchers. They said the technique could solve a diagnostic dilemma in patients with suspected colorectal cancer lesions that prevent them from undergoing conventional colonoscopy before surgery.
Of nearly 150,000 new colorectal cancer cases reported in the U.S. last year, obstruction occurred in approximately 16% to 23% of patients, said Michael Achiam, a research fellow and Ph.D. student at Copenhagen University Hospital in Herlev, Denmark.
"Only 10% of all large bowel obstructions are benign, but they still pose a problem because diagnosis can be difficult and biopsy might be inconclusive," he said at the 2008 International Symposium on Virtual Colonoscopy. "In the past 15 years MRI has shown that it's possible to differentiate benign from malignant tumors using the angiogenic capacity of the different tumors specifically, differentiating the fibrotic scar tissues of benign tumors from the neovascularity of malignant lesions as demonstrated in their contrast uptake."
 |
| Obstructing tumor detected at fast dynamic MR colonography. All images courtesy of Michael Achiam. |
While visual inspection can't answer the question of malignancy presurgically, he said, dynamic enhanced MRI has been used to distinguish benign from malignant lesions in several organs, including the bladder, lungs, breast, and even pulmonary nodules.
The researchers reviewed MRC data acquired over three years to assess whether the use of fast dynamic gadolinium-enhanced MRC could distinguish between benign and malignant colonic strictures, and to demonstrate the feasibility of visualizing the entire colon using MR colonography. The study included a group of patients with endoscopically diagnosed and biopsy-proven benign colon tumor stenosis, along with another group with biopsy-proven obstructive colon carcinoma, who were scheduled for surgery.
"We asked all patients with a known benign stenosis [n = 7] to participate, and we took the same number of patients with colon cancer," Achiam said.
Patients underwent purgative bowel cleansing or a fecal tagging regimen, ingesting 150 mL ferumoxsil plus 50 mL barium sulphate four times a day for two days prior to MRC.
Images acquired on a 1.5-tesla scanner (Achieva, Philips Healthcare, Andover, MA) included a T2-weighted balanced fast field-echo sequence, and a 3D T1 turbo field-echo (TFE) sequence following IV administration of 0.2 mL/kg of the contrast agent gadoterate meglumine. A postcontrast scan was acquired approximately 75 seconds later.
Two experienced radiologists evaluated the images, assessing regions of interest in an artery, a tumor region representative of the tumor as a whole, and a tumor region with the highest signal, Achiam said. The regions of interest were analyzed for maximum relative enhancement, time to peak, wash-in, and wash-out. The researchers measured interobserver correlation (observer I versus observer II) and observer reproducibility (for observer I).
"We unfortunately only had seven benign tumor stenoses, but the results I think were excellent," he said. "We found that only the wash-in time and the washout time were significantly different between benign and malignant tumors [p < 0.01]."
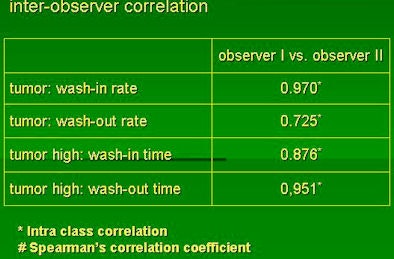
The researchers also found good correlation of results between the two observers and that colonic distension was adequate for a confident colon evaluation.
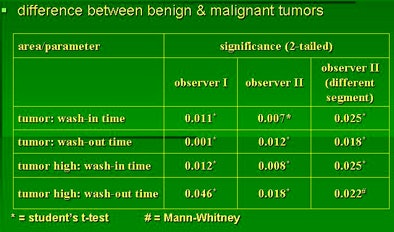 |
| The researchers analyzed regions of interest in an artery, the tumor overall, and the tumor region with the highest signal for maximum relative enhancement, time to peak, wash-in and wash-out. Both readers found that only the differences in wash-in values in the high-intensity area and the total tumor region for both patient groups (benign and malignant) were significantly different (above). Interobserver agreement was high (below). |
 |
"This study has shown that it is feasible to differentiate between malignant or benign tumors using fast dynamic gadolinium-enhancement MRC," Achiam said. "There is a significant difference in wash-in and wash-out time between malignant and benign tumor."
The fact that two observers found a significant difference in the same colonic segment with high correlation, and that a single observer found significant differences in different segments, suggest that the method is reproducible, he added.
Nearly a third of individuals older than 60 years and 7% of all symptomatic cases of diverticular disease result in obstruction and a clinical problem, Achiam said. Tumor ingrowth and adhesions can make it difficult to visualize the colon, and endoscopy can be painful and risky for the patient, he said. Once the colon becomes stiff and necrotic, there is a heightened risk of complications or bleeding from endoscopy. And the presence of necrotic tissue can also result in a false-negative biopsy, he said.
More to the point, when a tumor is obstructing it can be difficult to advance the scope beyond it and complete the exam, Achiam said.
"What appears to be a benign tumor is actually up to 15% to 20% of the time a malignant tumor that [endoscopy] can't reach," he said. "Incomplete colonoscopy due to colon obstructions are very common; up to 45% to 50% of cases have been reported, and synchronous cancers can be very important" as they've been shown to alter the surgical plan in 11% to 44% of cases, he said.
"I recommend a full preoperative evaluation by either MR or CT colonography in all patients," Achiam said. "If we can use this method to diagnose a colon tumor, we'll have better diagnostic ability, better patient information, and we'll have better surgical planning."
By Eric Barnes
AuntMinnie.com staff writer
January 16, 2009
Related Reading
Patients show slight preference for MR colonography over colonoscopy, June 6, 2007
MR colonography disappoints in reduced-prep protocol, March 6, 2007
MR colonography reveals significant extracolonic findings, February 14, 2007
Study pits CT against MRI for virtual colonoscopy, August 23, 2006
MR spectroscopy aids breast cancer diagnosis, June 8, 2006
Copyright © 2009 AuntMinnie.com