
If virtual colonoscopy is to function effectively as a screening tool, it must not only deliver consistently high sensitivity for clinically relevant lesions, but also show a low number of false positives and a high degree of concordance with optical colonoscopy.
Fortunately, virtual colonoscopy (also known as CT colonography or CTC) appears to be keeping its end of the bargain, according to Dr. Steven Wise, who led a study to calculate the positive predictive value of VC in nearly 1,000 individuals referred for polypectomy after a positive VC scan.
"The key finding of our study was that the positive predictive value of CTC for polyps 5 mm or larger is 91.6% -- that means a polyp called at CTC will be found at optical colonoscopy more than 90% of the time," said Wise, a radiology resident from the University of Wisconsin at Madison.
Wise spoke with AuntMinnie.com about the retrospective study before presenting it at the American Roentgen Ray Society (ARRS) meeting being held this week in Boston.
Because only a small percentage of individuals screened with VC go on to colonoscopy and polypectomy, sensitivity and specificity can't be measured in routine clinical practice, Wise said.
But the positive predictive value (PPV) of CTC is an important parameter that can be measured in a screening setting, providing quality metrics for the exam as well as comparisons between different institutions and groups of screening subjects that use VC, he said.
Measuring PPV "is detecting our ability to determine when we call a lesion -- is it really there?" he said. "PPV is something that you can measure in a clinical practice for CTC."
Wise, along with University of Wisconsin colleagues Dr. Perry Pickhardt and Dr. David Kim, measured PPV for the detection of polyps ≥ 6 mm found at screening CTC, and to assess the impact of polyp size, morphology, and diagnostic confidence on PPV.
They examined 5,124 consecutive adults (2,792 women, 2,332 men; mean age, 56.9 years) who underwent CTC screening between 2004 and 2008. Imaging followed a cathartic bowel cleansing and CO2 insufflation of the colon (ProtoCO2L, Bracco Diagnostics, Princeton, NJ).
Most subjects were prepped with a double dose of magnesium citrate the day before the exam. All subjects also ingested a 2% barium solution for stool tagging with meals and sodium diatrizoate to tag fluid, and they followed a clear liquid diet the day before imaging.
"We currently use magnesium citrate instead of sodium phosphate as our default laxative," Wise said. "Of note, many of the patients in my study were prepped with sodium phosphate."
Images were acquired on 8- and 16-detector-row scanners (GE Healthcare, Chalfont St. Giles, U.K.) using a low-dose protocol, 1.25-mm collimation, and 1-mm reconstruction interval. Hybrid 3D/2D polyp detection with 2D confirmation review was performed on a workstation using V3D-Colon software (Viatronix, Stony Brook, NY).
A total of 639 (12.5%) of the 5,124 consecutive adults undergoing CTC screening at the University of Wisconsin Health Center were prospectively called positive for polyps ≥ 6 mm in diameter, consisting of 958 total lesions. Of these, 479 patients with 739 CTC-detected lesions were evaluated at subsequent optical colonoscopy or surgery; the remaining 219 lesions were enrolled in short-term CTC surveillance or did not undergo optical colonoscopy for other reasons and were therefore excluded from analysis.
The PPV was derived from both optical colonoscopy and surgical findings. A finding considered true positive at VC had to be present at optical colonoscopy or surgery; conversely, a false-positive was any lesion found at VC but not optical colonoscopy, Wise said.
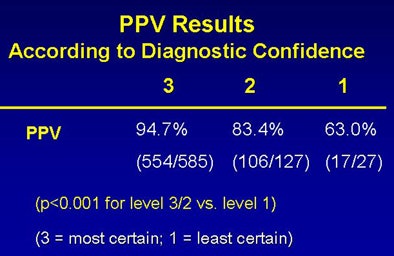
To be deemed a match, "the lesion size [at CTC] had to be within 50% of lesion detected at optical colonoscopy, and for a match in location, the maximum location had to be in the same or adjacent segment based on a six-segment model of the colon," Wise explained. Finally, the readers rated each polyp for diagnostic confidence, with 3 representing the most certainty about a finding, and 1 representing the least certainty.
The results showed a high concordance for CTC-detected lesions at subsequent optical colonoscopy, with an overall PPV greater than 90% for the screening program.
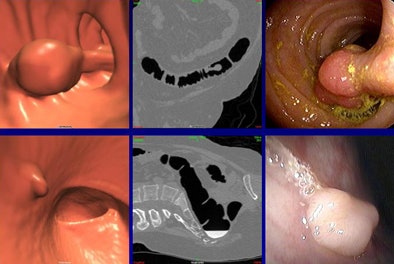 |
| Concordant findings included a 23-mm pedunculated lesion (top row), confidence level 3, that was seen on both 3D (upper left) and 2D (upper middle) views and confirmed at optical colonoscopy (upper right). Bottom row, a 6-mm sessile polyp (confidence level 3) was seen at both 3D (bottom left) and 2D (bottom middle) views and confirmed at colonoscopy (bottom right). All images courtesy of Dr. Steven Wise. |
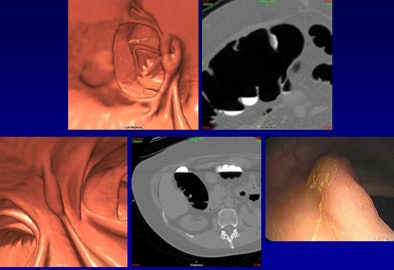 |
| Discordant findings included a 12-mm flat cecal lesion (top row) with contrast coating, diagnostic confidence 2, that was not visualized at optical colonoscopy. Bottom row, a 14-mm flat lesion (confidence level 3) was not seen at initial optical colonoscopy, but was confirmed at follow-up VC and optical colonoscopy. |
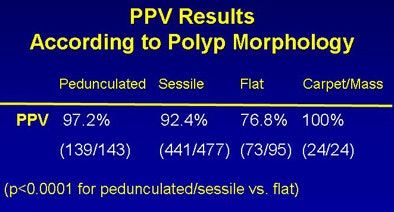
Increased diagnostic confidence and a polypoid (nonflat) morphology both correlated with a higher likelihood of finding a matching lesion at optical colonoscopy, while flat morphology reduced the likelihood of a match at optical colonoscopy, Wise said. Increased diagnostic confidence (level 3 > 2 >> 1) also correlated with a higher positive predictive value.
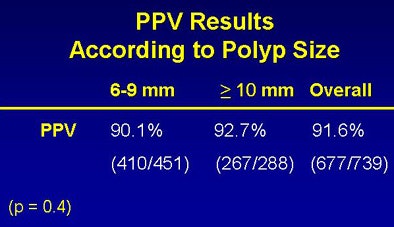 |
| The results based on polyp size show that overall PPV greater than 90% varied only slightly between 6- and 9-mm polyps and those 10 mm or larger (top). Below, results based on polyp morphology showed that PPV was higher for pedunculated and sessile polyps versus flat and carpet lesions. Bottom image, results based on diagnostic confidence showed that PPV was significantly higher when the diagnosis was more confident. |
 |
 |
The results further strengthen the argument that VC will be an effective screening test for colorectal cancer, Wise said.
"We can feel confident when they're performing optical colonoscopy that the lesion we called on CTC will actually represent a polyp when they get in there to perform optical colonoscopy," he said. "The lesion will [also] be in the same region and the same size as we called, so that optical colonoscopy can be optimized as a therapeutic test for detecting colorectal polyps and cancer."
"That's the major thing -- if people are calling polyps at CTC and the optical colonoscopists get in there and aren't finding anything, they're going to be reluctant to use CTC as a first-line test," Wise said.
By Eric Barnes
AuntMinnie.com staff writer
April 30, 2009
Related Reading
VC CAD plus 3D improves sensitivity for novice readers, April 21, 2009
Need for VC colon screening trumps physician turf battles, January 20, 2009
Image tools cut false positives in unprepped VC, August 4, 2008
VC CAD improves results for readers at all levels, April 7, 2006
VC holds up against back-to-back colonoscopies, July 19, 2005
Copyright © 2009 AuntMinnie.com




















