
For flat lesions detected at virtual colonoscopy, measuring the longest single dimension at 3D appears to minimize interobserver variability compared to 2D methods, according to a new study. Still, variability between two readers remained small using all methods, and the study concluded that applying a single measurement technique consistently is the most important factor in boosting observer agreement.
Flat lesions can be difficult to detect at virtual colonoscopy (also known as CT colonography or CTC), potentially resulting in false-negative interpretations, wrote Dr. Antonella Lostumbo, Dr. Abraham Dachman, and colleagues from University of Chicago Hospitals. And unfortunately, they wrote, there is little evidence to indicate whether flat lesions are better measured on 2D or 3D endoluminal views. In addition, the reading method and optimal window and level settings have yet to be optimized.
The researchers used a large clinical trial to compare 2D and 3D reading methods to see which is best for flat lesion measurement, as well as to determine which method is most reproducible. They published their results online before print in Academic Radiology (September 7, 2009).
"The reproducibility of lesion measurement is particularly important for patients with small colonic lesions (< 10 mm) because a small increase in size of a 6- to 9-mm lesion might prompt a decision for immediate optical colonoscopy rather than continued follow-up CTC," Lostumbo and colleagues wrote.
The study analyzed 88 colorectal lesions (≥ 6 mm) in 66 patients from a previously published clinical trial. Thus, the lesions were reviewed retrospectively, and polyps were measured to determine if they fit definitions of flat or sessile polyps. Sessile lesions were included because they were classified as such by visualization alone and had the potential to fit a particular definition of a flat lesion, the authors explained.
Eighty of the lesions were called sessile polyps, four were sessile/flat, five were flat, and polyp type was not available for five, they wrote. All lesions included in the analysis matched the criteria of "height" (≤ 3 mm high) or "ratio" (height ≤ half of the long axis). A subset of lesions was subject to inter- and intraobserver variability analysis.
Lesions missed by readers in the original trial were included in this analysis if they were visible in retrospect on at least one CTC view. Each polyp was viewed using four methods, including one for the 3D endoluminal view and three for 2D images based on different window (W) and level (L) settings. Lesion conspicuity was rated on a scale of 0 (not visible) to 4 (highly visible with discrete borders).
Flat lesions found in either supine or prone views were counted as a single dataset. Two fourth-year medical students, fully trained in CTC interpretation by an expert, each read all of the datasets.
The first reader evaluated 3D lesion conspicuity and measurements on a workstation using Vitrea 2 software, version 3.9 (Vital Images, Minnetonka, MN), with default ("fat-musclebone") settings. The 2D images were viewed with three tailored window/level settings including "lung" (W = 1500, L = -200), "flat" (W = 970, L = 87), and "soft-tissue" (W = 400, L = 10) settings.
The group found that using the "height less than half the length" criterion for flat polyps led to more datasets being classified as flat in 2D flat (n = 76), 2D soft-tissue (n = 82), and 3D (n = 73) views than in the 2D lung view (n = 49).
However, if long-axis length was used as the key metric for defining a flat polyp, the endoluminal 3D view (12.1%) significantly showed the least interobserver variability compared to lung (18.9%) or soft-tissue (20.2%) views. Meanwhile, 3D won the competition for conspicuity, the authors noted.
Lesions were significantly more conspicuous in the 3D view (2.9) when compared to 2D lung (2.5, p = 0.003), 2D soft-tissue (2.4, p < 0.0001), or 2D flat (2.5, p = 0.0029) views, Lostumbo and colleagues reported. No statistically significant difference in conspicuity was seen among any of the three 2D window/level settings.
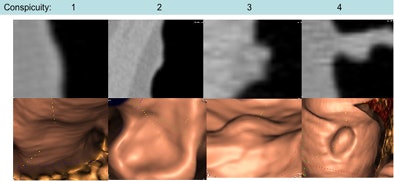 |
| Varying conspicuity on a scale of 1 (not visualized) to 4 (well visualized) is seen in 2D (top) and 3D (bottom) views of four polyps fitting the flat-polyp definition of height less than half of the long-axis length. Images courtesy of Dr. Abraham Dachman. |
In lesion measurement, there was no significant difference in the average percent difference in intraobserver long-axis measurements among the 2D lung (5.8%), 2D soft-tissue (6.1%), 2D flat (5.7%), and 3D endoluminal (7.5%) viewing methods (p = 0.63).
However, the average size difference (%) was significantly greater in intraobserver height measurements in the 3D endoluminal view (18.6%) compared to the 2D lung (8.9%), 2D soft-tissue (11.5%), and 2D flat (12.4%) viewing methods (p = 0.02).
Varying definitions of flat lesions are used throughout the literature, but it is important to use a consistent method to measure lesions because lesion size is considered the single most important factor in determining lesion detectability at CTC, the authors wrote.
"Differences in measurements between observers or within observers are important if the size of the lesion is being followed over time," they wrote. "There is no guarantee that the same person is going to read the same case. Therefore, interobserver variability is more important. The long-axis measurement in the 3D endoluminal view had the lowest interobserver variability."
And variability was low in long-axis measurements in all views when performed by the same observer. To minimize interobserver variability (such as when following a patient over time), the authors proposed using the single longest dimension at a 3D view as the key metric.
The study limitations include a small sample size, the use of older imaging equipment in the original clinical trial data, and the retrospective design.
"Despite these limitations, we were able to show robust differences between viewing methods and suggest the best measurement technique for flat lesions," they concluded, adding that more research is needed using a prospective study design.
By Eric Barnes
AuntMinnie.com staff writer
September 16, 2009
Related Reading
Virtual colonoscopy CAD improves flat-lesion detection, June 5, 2009
VC's high positive predictive value important for colonoscopy follow-up, April 30, 2009
Minimal-prep VC may miss more flat lesions, April 17, 2008
Flat colorectal tumors relatively common in U.S. population, linked to cancer, March 5, 2007
Prepless VC misses some diminutive flat lesions, January 17, 2006
Copyright © 2009 AuntMinnie.com




















