This fall, as the world awaits a vaccine to stave off H1N1 and hopes for the best, radiologists are finding that thoracic CT can aid early identification of the influenza known commonly, if inaccurately, as swine flu. A new paper in the American Journal of Roentgenology shows how CT detected a case that had shown a false-negative result on an H1N1 rapid antigen test.
Most cases of the H1N1, which is not known to be transmitted by pigs, are self-limiting. However, a number of fatal cases in recent months have raised questions about H1N1's virulence, and radiology's potential role in early detection, researchers report in the upcoming December issue (AJR online, December 2009, Vol. 193).
Dr. Daniel Mollura from the National Institutes of Health's Clinical Center in Bethesda, MD, along with colleagues from Flushing Hospital Medical Center in Flushing, NY, Weill Cornell Medical College in New York City, and two other institutions, report on the use of CT in a fatal case of H1N1 influenza.
"Epidemiologic data to date suggest that the newly emerged H1N1 virus, although transmissible from person to person, is of relatively low virulence. However, as in the case of seasonal influenza, even an agent with low pathogenicity for healthy children and adults can still cause lethal disease in young infants, pregnant women, elderly individuals, and persons with immune deficiency or other chronic medical conditions," Mollura et al wrote.
Early recognition is therefore essential, particularly in high-risk groups, so that diagnostic tests, the initiation of antiviral therapy, and preparation for more intensive supportive measures as needed can be arranged, the authors wrote. To this end, "the role of radiologic imaging in epidemic detection and response is evolving, with imaging being used as a tool for identifying severe cases," they wrote.
The patient
A previously healthy middle-aged man presented to the emergency department with a five-day history of fever, fatigue, nausea, diarrhea, and intermittent cough. The patient was a nonsmoker who said he did not use recreational drugs. Head CT at admission was normal.
"Admission vital signs included a fever of 103.3°F, blood pressure of 92/53 mm Hg (systolic/diastolic), pulse of 84 beats per minute, respiration of 22 breaths per minute, and oxygen saturation of 95% on bilevel positive airway pressure (BiPAP) ventilatory support," the authors reported. His white blood cell count was 10,600 cells/mm3, and serology was unremarkable. The patient underwent a physical exam for confused mental status, bibasilar pulmonary crackles on auscultation, and obesity.
Imaging included portable chest x-ray, which showed peripheral patchy opacities, followed by chest CT on day 1 of admission. CT was not used with contrast, or repeated, due to the severity of the patient's condition.
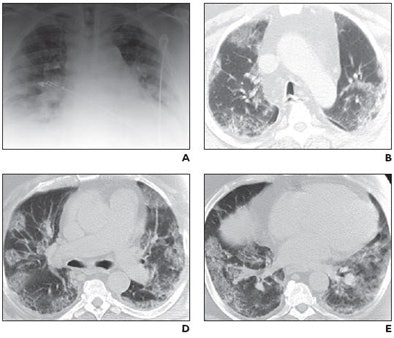 |
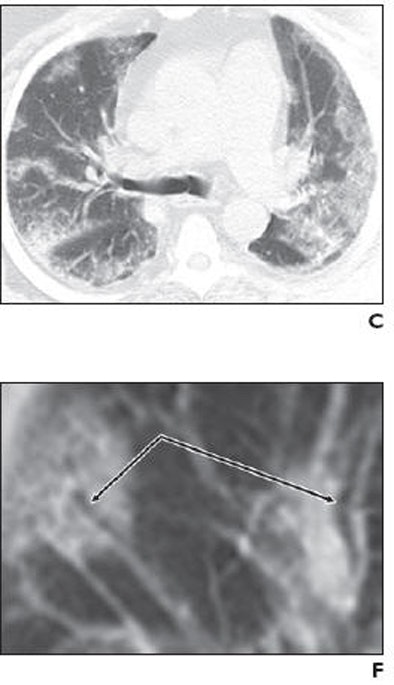
| Middle-aged man with no history of chronic pulmonary disease presented to emergency department with five-day history of fever, fatigue, nausea, diarrhea, and cough. Radiography and CT were performed. Unenhanced chest CT lung window images showed multifocal peripheral ground-glass opacities involving all lobes. Patient died on fifth day. Above: A, Chest radiograph obtained at clinical presentation shows peripheral opacities. B, Unenhanced chest CT lung window image shows apical patchy peripheral ground-glass opacities. D, Unenhanced chest CT lung window image reveals that lingula, right middle lobe, and both lower lobes show patchy, peripheral, rounded, peribronchial ground-glass opacities with air bronchograms. E, Unenhanced chest CT lung window image shows bilateral lung bases with ground-glass opacities still predominantly patchy at periphery, but more confluent ground-glass attenuation. Below: C, Unenhanced chest CT lung window image reveals that upper lobe and superior segments of both lower lobes show peripheral peribronchial ground-glass opacities. F, Magnified view of anterior segment of right upper lobe shows ground-glass opacity peripherally and air bronchograms (arrows). Images used with permission of the American Roentgen Ray Society. |
 |
In the hospital the patient continued to have severe hypoxia despite ventilation and was intubated later that day, receiving IV antibiotics, oseltamivir, and corticosteroids. Two H1N1 influenza rapid antigen tests (by nasal swab) were performed; both were negative.
"Many of the opacities showed air bronchograms with normal-sized bronchial airways leading into each rounded ground-glass focus, and most large airways showed no significant wall thickening or plugging," Mollura et al wrote of the CT findings. "The ground-glass opacities were located throughout the upper and lower regions of all lobes in a peribronchovascular distribution. CT showed no evidence of a mosaic perfusion pattern, suggesting no localized air trapping or regional changes in blood flow."
No centrolobular nodularity or tree-in-bud opacities were seen, suggesting an absence of small-airway inflammation in the secondary lobules. IV contrast media could not be given due to the patient's progressing renal failure, the group noted.
Chest CT in soft-tissue windows showed an absence of mediastinal lymphadenopathy, or pleural or pericardial effusion. Echocardiography showed "moderate concentric left ventricular hypertrophy and an ejection fraction of 58% with mild-to-moderate tricuspid regurgitation," they wrote.
Finally on day 2 a reverse transcriptase polymerase chain reaction (RT-PCR) test of a nasopharyngeal swab was found to be positive for H1N1 swine-origin influenza A virus. Hypoxia, renal failure, and acidosis continued to progress in hospital, and the patient died on the fifth day following admission.
A postmortem examination showed patchy regions of parenchymal discoloration in all of the lung lobes bilaterally, in agreement with the CT and radiographic evidence of multiple patchy air-space ground-glass opacities. Gross pathology showed no evidence of pulmonary emboli or infarction. Histologic examination of the lungs showed areas of intra-alveolar hemorrhage with fibrinous material, proteinaceous fluid, macrophages, and reactive pneumocytes in addition to RT-PCR and immunohistochemical confirmation of novel H1N1 infection.
"These pathologic findings are consistent with a primary influenza viral pneumonitis leading to diffuse alveolar damage and acute respiratory distress syndrome (ARDS) clinically, and correspond to the described imaging features showing severe injury to peribronchial spaces," they wrote.
The fatal case of H1N1 influenza A virus (S-OIV) revealed a pattern of rounded peripheral ground-glass opacities on CT that can also be seen on severe peribronchial air-space disease, but were shown radiographically to differ from cardiogenic edema.
"The findings were also suggestive of less airway inflammation than in other reported viral pneumonias," the authors reported.
"Early CT may help clinicians recognize incipient cases of severe influenza and improve our understanding of the pathogenesis of the disease," Mollura et al wrote. "Further collection of radiographic data and pathologic-radiologic correlation are warranted."
By Eric Barnes
AuntMinnie.com staff writer
October 14, 2009
Related Reading
Virus outbreaks put scrutiny on infection control practices, August 10, 2009
Survey: MRI centers lack infection control, May 28, 2009
U.S. FDA warns against wearing skin patch during MRI, March 6, 2009
11 steps for preventing MRSA infections in MRI, November 6, 2008
Copyright © 2009 AuntMinnie.com




















