
A technique that analyzes the attenuation of small regions of interest in the bowel wall at CT can improve the diagnosis of suspected bowel wall ischemia, a condition associated with substantial morbidity and mortality.
Close to 10% of patients with small-bowel obstruction have strangulating obstruction, a condition that requires surgery as soon as possible to avoid a mortality risk as high as 25%, explained Kyung Mi Jang from Hallym University College of Medicine in Anyang-city, Korea, and colleagues in the April American Journal of Roentgenology.
CT is the method of choice for diagnosing obstruction, and lack of bowel wall enhancement is the modality's most specific sign, they noted. But diagnosing ischemia can be difficult due to the thinness of the lesions and the bowel wall, particularly when transmural infarction is present, making it difficult to assess CT attenuation. The authors hoped to improve CT's diagnostic accuracy for bowel wall obstruction by combining visual assessment with CT attenuation information.
"We thought that when a region of interest (ROI) is drawn across the bowel wall while avoiding adjacent mesenteric vessels, bony structures, high-attenuated mesenteric fluid, and other high-attenuated structures or lesions that are denser than the bowel wall, the maximal attenuation of the ROI could reflect the bowel wall attenuation," they wrote (AJR, April 2010, Vol. 194:4, pp 957-963).
The retrospective study sought to evaluate CT's performance in diagnosing intestinal ischemia, using the maximal attenuation ROIs.
The researchers looked at CT scans of 60 patients with small-bowel obstruction, classifying the reference standard of the clinicopathologic groups into four categories: no bowel necrosis, mucosal-submucosal necrosis, superficial muscle necrosis, and transmural necrosis.
In all, 35 of the patients underwent small-bowel resection for intestinal ischemia or unreleased bowel from adhesion. Adhesiolysis without bowel resection was performed in 20 of the remaining patients. Partial small-bowel obstructions were confirmed in five patients (8.3%), complete small-bowel obstruction in26 (43.3%), and closed small-bowel obstruction in the remaining 29 patients (48.4%).
Both unenhanced and contrast-enhanced scans (120 mL iohexol, Omnipaque 300, GE Healthcare, Chalfont St. Giles, U.K.) were obtained in all patients using a 16-detector-row CT scanner (Mx8000 IDT, Philips Healthcare, Andover, MA). The settings included 1.5-mm collimation, reconstruction increment of 1 mm, and pitch of 1.2. Then 5-mm-thick transverse and 4-mm-thick coronal sections were reconstructed for evaluation.
Using methodology based on a literature search, the authors classified CT results into one of five categories using a five-point scale:
- CT findings of no ischemia
- Equivocal CT results
- "Possibly intestinal ischemia" indicated that lesions with two or more of the assessed CT findings were present
- "Probably intestinal ischemia" indicated the presence of lesions with reduced enhancement of the bowel wall on contrast-enhanced CT, and at least one of the following: mural thickening, vascular engorgement, mesenteric haziness, or ascites
- "Definitely intestinal ischemia" indicated that lesions were present, there was absent or reduced enhancement of bowel wall on contrast enhancement, and there was the presence of pneumatosis intestinalisor portomesenteric venous gas
The researchers measured the maximal attenuation of an ROI at selected obstructed small-bowel loops on contrast-enhanced and unenhanced CT scans, evaluating the diagnostic performance of the two methods by one-way analysis of variance and receiver operator characteristics (ROC) curve analysis.
Pathologic analyses of the resected small bowel in 35 patients showed five cases (14.3%) of no bowel necrosis, 10 cases (28.6%) of mucosal/submucosal necrosis, eight cases (22.9%)of superficial muscle necrosis, and 12 cases (34.2%) of transmural necrosis.
All 19 cases with a visual assessment score of 1 or 2 ("definitely" or "probably") for intestinal ischemia were in the "no bowel necrosis" group or "mucosal-submucosal necrosis" group. Of the 13 cases with a score of 3, there were no cases of transmural necrosis at pathologic analysis.
Thus, the sensitivity, specificity, positive and negative predictive values, and accuracy of visual assessment for intestinal ischemia were 91.7% (33/36), 66.7% (16/24), 80.5% (33/41), 84.2% (16/19), and 81.7% (49/60), respectively, the authors reported.
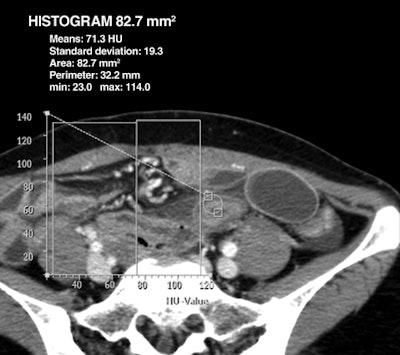 |
| Woman, 39 years old, with small-bowel obstruction secondary to adhesion. Axial contrast-enhanced (above) and unenhanced (below) CT images through lower abdomen show thickened small bowel with preserved bowel wall enhancement and perilesional mesenteric haziness. Maximal attenuation of ROI on contrast-enhanced CT image above is 114 HU, and subtraction value of maximal attenuation of ROI between contrast-enhanced (above) and unenhanced (below) images is 60 HU at thickened bowel lesion. At surgery, peristalsis and arterial pulsation of bowel were preserved, and there was no bowel lesion of discoloration. Images republished with permission of the American Roentgen Ray Society. |
 |
The maximal attenuation of the ROIs at contrast-enhanced CT and the subtraction value between the maximal attenuation on contrast-enhanced CT and that on unenhanced CT scans at selected bowel loops differed significantly according to clinicopathologic group (p < 0.001). Overall, the attenuation method did a little better.
"The area under the ROC curve of the maximal attenuation subtraction values between contrast-enhanced and unenhanced CT scans (0.995) was higher than that of visual assessment (0.908) for the detection of intestinal ischemia," the authors wrote.
"In several articles, investigators have reported that the CT findings suggestive of intestinal ischemia individually are insufficiently sensitive, but that a combination of CT findings increases the accuracy of CT in the diagnosis of intestinal ischemia," they wrote.
Unenhanced CT images are not generally acquired at most institutions in the emergency setting to reduce radiation dose; however, the study results suggest that "unenhanced CT has a useful role in the assessment of bowel wall attenuation and that using only the maximal attenuations of ROIs on contrast-enhanced CT scans for the diagnosis of intestinal ischemia was less accurate than the visual assessment for the diagnosis of intestinal ischemia," Jang and colleagues wrote.
When the diagnostic criterion for intestinal ischemia was a visual assessment score of greater than 2 or a maximal attenuation of an ROI on contrast-enhanced CT scans of less than 60 HU, sensitivity of visual assessment was as high as 97.2%.
The overall sensitivity of visual assessment in this study, as high as 91.7% (positive predictive value, 80.5%; negative predictive value, 84.2%; accuracy, 81.7%) for disease scored greater than 2, was comparable to that of other studies.
Meanwhile, the maximal attenuation of an ROI on contrast-enhanced CT scans of less than 60 HU, which was the approximate mean value of the mucosal-submucosal necrosis group, demonstrated a sensitivity of 52.8%, specificity of 83.3%, positive predictive value of 82.6%, negative predictive value of 54.1%, and accuracy of 65.0% for diagnosing intestinal ischemia.
The authors noted several limitations of the study, including its retrospective nature, the difficulty of assessing the exact same location on the bowel wall at both enhanced and unenhanced scans, and the lack of test bolus imaging that would have improved the reliability of attenuation measurements, to name a few.
Using maximal attenuation of an ROI was a reliable and useful method for diagnosing intestinal ischemia and showed good correlation with pathology results, the authors concluded.
By Eric Barnes
AuntMinnie.com staff writer
April 19, 2010
Related reading
MRI enterography shows shortcomings for Crohn's disease, February 23, 2010
CT finds differences in omental infarction between children, adults, January 3, 2007
3D reveals what axial images can't in small-bowel CT, November 15, 2006
CT differentiates mesenteric ischemia from transmural necrosis, January 3, 2006
Success begets growing role for CT enteroclysis, November 18, 2004
Copyright © 2010 AuntMinnie.com




















