Evaluating pancreatic CT images to determine resectability is one of the more difficult jobs in radiology, perhaps more so because the stakes are so high. But a lot of mistakes can be avoided with 3D imaging and careful attention to a few details.
At the 2010 International Society for Computed Tomography (ISCT) meeting, Elliot Fishman, MD, from John Hopkins University in Baltimore offered some tips on identifying even the smallest pancreatic masses while weeding out the impostors.
Pancreatic masses are pretty easy to miss -- particularly if they're small or located in the head or tail of the organ, he said. Sometimes they can be appreciated only indirectly, such as when a pancreatic duct is dilated. And it's pretty easy to mistake another finding for a pancreatic tumor.
John Hopkins Medicine knows a thing or two about the subject, with its center dedicated to pancreatic cancer, a place where patients undergo a comprehensive analysis and treatment that includes imaging, radiation therapy, medical therapy, surgery, and pathology services. Over the years, the center has generated a lot of data on patients with pancreatic cancer, publishing more than one report on the findings.
One such report, on common misdiagnoses in the abdomen, found that 18% of patients with pancreatic cancer get their final diagnosis based on imaging findings. Overall, 48 of 203 patients, or 23.6%, had a change in management based on a clinical review of their case by a multidisciplinary tumor board, Fishman said of the report (American Journal of Roentgenology, March 2010, Vol. 194:3, pp. 660-667).
Another Hopkins paper found a high rate of changed diagnoses when both internal and outside CT scans were reviewed at the university, Fishman said.
For example, initial CT reports described locally advanced or unresectable disease in 34.9% of patients, metastatic disease in 17.7%, and locally advanced disease with metastasis in 1.1%. But review of the imaging results (both outside and in-house scans) produced a change in the status of the patient's clinical stage in 38 of 203 (18.7%) patients (Annals of Surgical Oncology, August 15, 2008, Vol. 15:8, pp. 2,078-2,080).
"If you look at the pancreatic tumor, the first thing is detectability," Fishman said. "At the end of the day, if you don't detect the tumor, you're not going to be able to be specific as to what it is you're doing with staging."
When an adenocarcinoma is missed, the most common reason is that it's simply too small to see on CT, but there are other causes as well, he said.
Perhaps a lesion is visible but not appreciated because it's more of a textural change than a discrete mass, Fishman said. Maybe there is only a dilated pancreatic duct or common bile duct without a discrete mass. But a dilated duct without an apparent mass should never be ignored, he said.
"If you see a dilated duct, there has to be a lesion present," Fishman said. If you don't see it, maybe do another study."
 |
| Patient has dilated pancreatic duct, but no tumor is visible. All images courtesy of Elliot Fishman, MD. |
The goal these days, of course, is to detect lesions at an earlier point when they are resectable, he said, adding that resectability is not a function of tumor size.
"Even the smallest lesions can have spread to the vessels to make them unresectable," he said.
Islet cell tumors are another challenge, according to Fishman. These tumors are small and often overlooked, and while scanning is done in the venous phase, lesions are seen only in the arterial phase. Finally, islet cell tumors are difficult to appreciate because they do not distort the pancreatic outline, he said.
Whether or not an islet cell tumor is detected tends to be related to CT technique, Fishman said.
"Islet cell tumors -- some of the larger ones as well as the small ones -- are very vascular on the arterial phase," he noted. But within 30 seconds they become isodense and hard to distinguish from the surrounding parenchyma.
 |
| A splenic artery aneurysm mimics an islet cell tumor. |
On the other hand, any number of potential errors can result from calling something else a pancreatic mass, Fishman said. Common mistaken findings include:
- Peripancreatic mass that simulates a pancreatic tumor
- Duodenal carcinoma
- Gastrointestinal stromal tumor (GIST)
- Peripancreatic nodes
- Lymphoma
"It's very easy to make mistakes, particularly by the head of the pancreas and the tail of the pancreas," he said. For example, a splenic artery aneurysm can easily be misdiagnosed as an islet cell tumor or a splenule, he said.
"Splenic lesions very much at times simulate pancreatic masses; it's a very difficult area," Fishman said. You have to look at arterial and venous phase enhancement, he said. One clue is that enhancement of the splenic artery is significantly matched with that of the spleen.
Findings involving the splenic artery, particularly if the artery is very tortuous, can easily simulate distal pancreatic lesions, Fishman said.
Metastatic tumors of the pancreas, particularly renal cancers, are especially vascular on arterial-phase imaging, but these, too, quickly become isodense, he said.
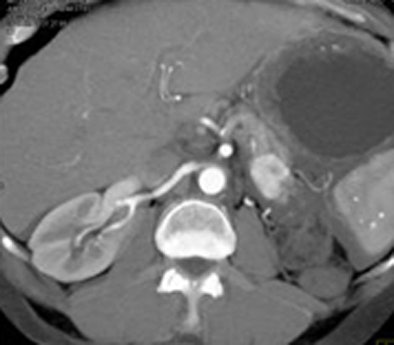 |
| A renal cell carcinoma metastasis to the pancreas is seen only on arterial-phase CT. |
In one case, a GIST tumor was misdiagnosed as a pancreatic mass. "If you don't see a dilated common duct, and you don't see a dilated pancreatic duct, and you have a reasonably sized lesion, then it's not pancreatic," he said.
A number of pitfalls can occur in CT imaging of patients with suspected pancreatic masses, but errors can be avoided, Fishman said.
"I think using multiphase imaging analysis of 3D mapping, and awareness of the pitfalls, particularly around the head and tail of the pancreas, will help minimize potential errors," he said.
By Eric Barnes
AuntMinnie.com staff writer
July 22, 2010
Related Reading
IORT shows promise as pancreatic cancer treatment, July 13, 2010
HIFU for liver, pancreatic cancer has high complication rate, July 12, 2010
Diffusion-weighted MRI may help detect autoimmune pancreatitis, March 23, 2010
Pre-, postcontrast DWI-MRI similar in liver, spleen, and pancreas, May 18, 2009
Chemoradiation after pancreatic surgery adds months to survival, January 28, 2010
Copyright © 2010 AuntMinnie.com