
There's no need to acquire images during both stress and rest phases in dual-energy CT (DECT) myocardial perfusion imaging, say researchers from the U.S. and Germany. A stress phase combined with a delayed-enhancement phase performs just as well while reducing radiation dose by a third.
The two-phase study also cuts the exam time for CT-based myocardial perfusion imaging, said Thomas Henzler, MD, from the Medical University of South Carolina (MUSC) in Charleston and Heidelberg University, in Mannheim, Germany, in a presentation at the 2010 RSNA meeting last month.
Hemodynamic significance
Multiple studies have shown high accuracy for 64-detctor-row CT and dual-energy CT in detecting coronary artery stenosis. What coronary CT angiography (CTA) can't provide, however, is information about the hemodynamic significance of the detected stenosis, Henzler said.
"DECT coronary angiography allows us to visualize the coronary arteries, evaluate myocardial function, and also by displaying and selectively visualizing the iodine distribution within the myocardium, assess perfusion defects within a single scan," Henzler said. Initial studies have shown high accuracy and diagnostic performance for standard rest DECT compared to SPECT myocardial perfusion imaging.
"The purpose of our study was twofold: First, we wanted to evaluate a combined rest/stress and delayed-enhancement DECT protocol compared with SPECT, and then [we wanted to] compare SPECT with the same exams using only adenosine stress images and delayed-enhancement DECT," he said.
Henzler, along with MUSC's Joseph Schoepf, MD, and colleagues in Germany and South Carolina, scanned 57 patients (46 men, 11 women; mean age, 62 years ± 10). The imaging protocol included electrocardiogram-gated three-phase contrast-enhanced DECT (Somatom Definition Dual Source, Siemens Healthcare, Malvern, PA) with adenosine-stress, rest, and delayed-enhancement imaging.
Patients received 80 mL of iopamidol (370 mgI/mL Isovue, Bracco Diagnostics, Princeton, NJ) followed by a 50-mL saline flush at 6 mL/sec. Patients received 140µg/min/kg adenosine under physician supervision for the stress scan, Henzler said.
Retrospectively gated DECT studies were acquired during peak adenosine stress, at rest, and six minutes after the last contrast injection. Tube settings for the dual-source scanner were 140 mAs/rotation at 140 kV for tube A and 165 mAs/rotation at 100 kV for tube B, at 2 x 64 x 0.6 mm for the rest scan and 2 x 64 x 1.5 mm for the stress and delayed-enhancement scan
DECT datasets were used to map myocardial iodine distribution within the left ventricular myocardium. Myocardial segments were classified as normal, showing reversible ischemia, or as fixed perfusion defects.
"If there was no perfusion defect on stress, rest, or delayed-enhancement DECT, those segments were classified as normal," Henzler said. "If we found perfusion defect only on rest images without delayed enhancement, we classified those defects as reversible ischemia, and if there was evidence of perfusion defect on rest scan stress and on stress with delayed-enhancement images, we classified those defects as fixed perfusion defects."
The team performed a segmental analysis of the results based on a combination of stress, rest, and delayed-enhancement DECT, as well as using a combination of stress-only and delayed-enhancement DECT. Finally, the researchers compared the results of stress/rest plus delayed enhancement versus SPECT to stress plus delayed enhancement versus SPECT.
According to the results, perfusion defects were detected in 214 of the 969 myocardial segments analyzed at rest DECT, and 227 of 969 segments on adenosine stress DECT studies, they reported. Delayed-enhancement DECT showed perfusion in 175 of 969 myocardial segments.
Rest DECT confirmed rest SPECT findings with 92.1% sensitivity, 96.4% specificity, and 96.5% accuracy. Stress DECT confirmed stress SPECT findings with 94.6% sensitivity, 97.5% specificity, and 96.8% accuracy, Henzler said.
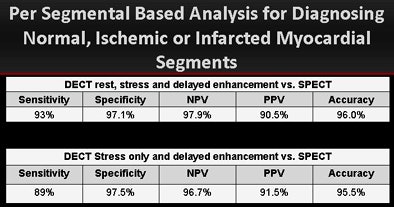 |
| Per-segment analysis, above, and per-patient analysis, below, for the diagnosis of normal, ischemic, or infarcted myocardial segments shows equivalent accuracy for stress plus delayed-enhancement DECT versus stress/rest plus delayed-enhancement CT versus SPECT for the detection of myocardial infarction. All images courtesy of Thomas Henzler, MD. |
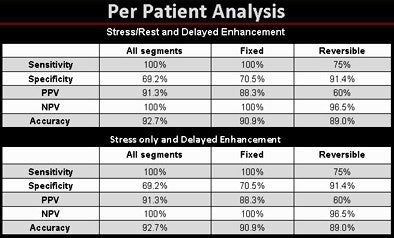 |
"On a per-segment basis it was interesting to see we had high sensitivity and diagnostic accuracy compared to SPECT," he said. "There was no difference on a per-patient analysis between stress and rest with delayed enhancement, [and no significant difference] between stress and delayed enhancement, for a patient-based sensitivity of 100% and diagnostic accuracy of 92% for both protocols."
The sensitivity, specificity, and accuracy of combined stress, rest, and delayed-enhancement DECT for diagnosing normal, ischemic, and infarcted myocardial segments were reported at 93%, 97.1%, and 96.0%, respectively. Stress-only DECT combined with delayed-enhancement DECT confirmed SPECT findings with 89% sensitivity, 97.5% specificity, and 95.5% accuracy.
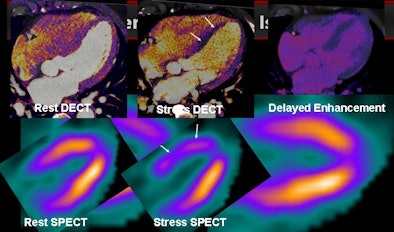 |
| Patient with normal tracer uptake on rest images and on SPECT stress shows minor tracer uptake in the intraventricular septum. At DECT there is homogeneous contrast media enhancement at the time the scan is performed in the left ventricle and myocardium. Adenosine stress scan shows minor perfusion of the intraventricular septum but no evidence of delayed enhancement, providing good correlation to SPECT findings. |
The radiation dose was approximately 13 mSv using the three-phase protocol, versus 6-8 mSv for the two-phase exam that skips the rest phase, Henzler told AuntMinnie.com in an e-mail.
In any case, Henzler said, patients who stand to benefit from late-phase myocardial perfusion assessment are not typically candidates for ultralow-dose high-pitch scanning used to examine individuals at low risk of coronary artery disease.
The higher-risk patients who are candidates for two-phase myocardial perfusion CT are receiving about 6-8 mSv of radiation, at least one-third less than the three-phase exam that includes the rest phase. The protocol also delivers significantly less radiation than the typical SPECT protocol, which delivers 11-13 mSv, he said.
By Eric Barnes
AuntMinnie.com staff writer
January 4, 2011
Related Reading
Turf battles may be impeding growth of CCTA compared to MPI, December 28, 2010
CAD boosts new readers in diagnosing stenosis on CCTA, November 10, 2010
Adenosine stress DECT equivalent to SPECT, MRI, November 21, 2008
Dual-source CT edges into cardiac SPECT turf, March 6, 2008
CTA predicts functional recovery of the myocardium, September 7, 2007
Copyright © 2011 AuntMinnie.com




















