Owing to its high resolution and wide anatomic coverage, dynamic first-pass perfusion 320-detector-row CT outperforms PET/CT for distinguishing benign from malignant lung nodules, researchers from Japan report in Radiology. The technique could potentially facilitate patient management by reducing the frequency of negative biopsies.
"Ideally, the goals of diagnosis and management are to promptly perform surgery in all patients with operable malignant nodules and to avoid unnecessary thoracotomy in those patients with benign lesions," wrote Yoshiharu Ohno, MD, PhD, and colleagues from Kobe University, Yamanashi University, and Toshiba Medical Systems in Radiology (February 2011, Vol. 258:2, pp. 599-609). "Therefore, the ability to distinguish benign from malignant nodules accurately and in the least invasive manner possible is essential."
Benign and malignant nodules are thought to have distinctly different physiologic, metabolic, and pharmacokinetic characteristics, and attempts to distinguish the two have been performed in a variety of ways, from CT to dynamic MRI to PET or combined F-18 FDG-PET/CT. According to the authors, dynamic wide-area CT may be well suited to detecting some unique properties of malignant nodules.
Nodule perfusion and extraction fraction values from dynamic first-pass 320-detector-row CT may help radiologists distinguish malignant from benign pulmonary nodules more effectively than the quantitative blood volumes calculated from the same data, as well as the FDG uptake assessment at combined PET/CT, the authors stated.
Although promising results have been reported with PET/CT and MRI, "a substantial portion of nodules detected with them are false negative and/or false positive," they wrote.
The prospective study aimed to assess the capabilities of quantitative first-pass perfusion 320-detector-row CT for distinguishing benign from malignant nodules compared to PET/CT.
The cohort included 50 consecutive patients (mean age, 73.3 years ± 8.6) with 76 pulmonary nodules (mean diameter, 15.9 mm ± 7.7; diameter range, 4-29 mm). All patients underwent dynamic area-detector CT, PET/CT, and microbacterial and/or histopathologic exams.
Dynamic area-detector CT examinations were performed with a 320-detector-row CT scanner (Aquilion One, Toshiba Medical Systems) using volumetric cine scanning without helical imaging.
Based on histopathologic results, the 76 pulmonary nodules in the cohort were categorized into three groups:
- Benign nodules with low biologic activity (n = 6)
- Benign nodules with high biologic activity (n= 27)
- Malignant nodules (n = 43)
The 43 malignant nodules consisted of 40 peripheral lung cancers (30 adenocarcinomas with mixed types of bronchioloalveolar carcinomas [BACs] and other subtypes, including acinar, papillary, or solid adenocarcinomas; five localized BACs; two adenocarcinomas without mixed subtypes; and three squamous cell carcinomas) and three metastatic lung tumors consisting of two colon cancers and one thyroid cancer.
The six benign nodules with expected low biologic activity consisted of four tuberculomas and two hamartomas. The 27 benign nodules with expected high biologic activity included 21 organizing pneumonias, four atypical Mycobacterium infections, one case of aspergillosis, and one case of cryptococcosis.
For each CT dataset, the authors calculated the perfusion in each nodule derived using the maximum slope model (PFMS). Then the extraction fraction was derived using the Patlak plot model (EFPP). Next, blood volume was calculated using the Patlak plot model (BVPP). Finally, the nodule parameters were compared statistically among the three nodule groups.
"Our study results show significant and reproducible differences in [maximal standard uptake value (SUVmax)] and in all of the evaluated dynamic first-pass area-detector CT indexes among the malignant nodules, benign nodules with expected low biologic activity, and benign nodules with expected high biologic activity," Ohno and colleagues reported. "In addition, dynamic first-pass area-detector CT enabled more specific and accurate differentiation between the malignant and benign pulmonary nodule groups than did PET/CT."
All indexes in the malignant nodule group were significantly different from those in the low-biologic-activity benign nodule group (p < 0.05). Areas under the receiver operator characteristics (ROC) curve for PFMS and EFPP were significantly larger than those for BVPP (p < 0.05) and SUVmax (p < 0.05).
Significant differences were also found between benign and malignant nodules in two dynamic area-detector CT indexes: PFMS and EFPP.
The specificity and accuracy of PFMS (79% and 90%, respectively) and EFPP (82% and 86%, respectively) were significantly higher than those of both blood volume (BVPP: 54% and 72%, respectively) and standardized uptake value (SUVmax: 52% and 74%, respectively) (p < 0.05).
Comparisons among all of the perfusion indexes evaluated by maximum slope and Patlak plot analyses of dynamic wide-area CT and PET/CT SUVmax data revealed significant correlations with each other. And the reproducibility coefficients for all of the indexes evaluated in the study were consistent with those of previous studies, the group noted.
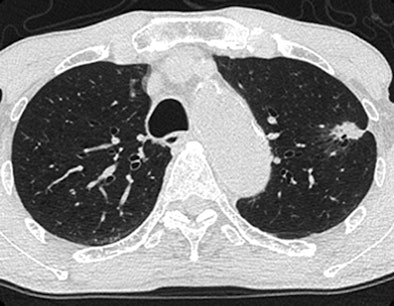 |
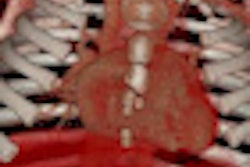
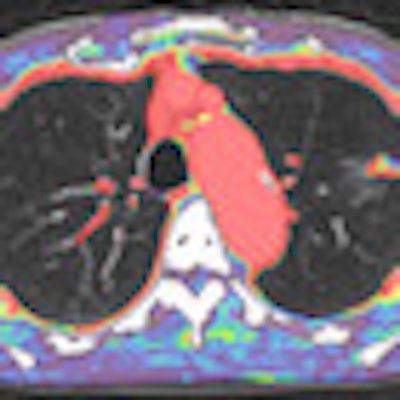
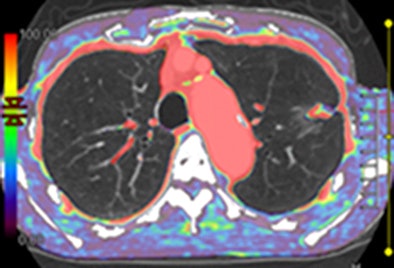
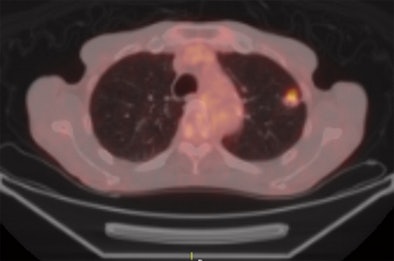
| Axial images of primary lung cancer (adenocarcinoma) in left upper lung lobe in 76-year-old man. Above, thin-section CT image shows nodule 18 mm in diameter in left upper lobe. Below, perfusion map shows nodule has high perfusion, with PFMS (scale at left) determined to be 89.9 mL/100 mL/min; this is a true-positive case according to maximal slope method results. Bottom, integrated PET/CT image shows high uptake of FDG, with SUVmax of lesion determined to be 3.8, indicating a true-positive case. Images republished with permission of the Radiological Society of North America from Radiology, February 2011, Vol. 258:2, pp. 599-609. |
 |
 |
The correlations held for every measurement parameter and every nodule type. All 320-detector-row wide-area CT indexes, as well as SUVmax, were significantly different from the malignant nodules, both including and excluding bronchoalveolar-cell carcinomas and benign nodules with expected low biologic activity, Ohno and colleagues reported.
"Comparisons of the diagnostic capability of the dynamic area-detector CT indexes and the SUVmax demonstrated that PFMS and EFPP enabled significantly more specific and accurate differentiation than did BVPP and SUVmax," Ohno and colleagues wrote. "These results suggest that dynamic area-detector CT with use of blood flow parameters such as the PFMS and EFPP rather than the BVPP in a nodule can be used to more precisely and accurately analyze an increase in tumor angiogenesis, which induces tumor perfusion and microvascular density, the extracellular space and permeability surface of capillaries, and the extraction fraction of malignant tumors."
They credited use of 320-detector-row dynamic first-pass CT to enabling more specific and accurate differentiation between the malignant and benign pulmonary nodule groups than PET/CT. The wide-area CT system can also be used to evaluate time-attenuation curves for several pulmonary nodules located within a 16-cm area and in the main trunk of the pulmonary artery, important for quantitative analysis of the blood flow pattern with use of maximum slope and Patlak plot methods at the same time.
Significantly moderate correlations were found between the dynamic area-detector CT indexes and the SUVmax measurements. These blood-flow parameters can improve precision and accuracy in distinguishing benign from malignant nodules compared to FDG uptake assessment "because they show enhanced expression of glucose transporter messenger RNA to result in an increase in glucose transport protein in malignant tumors," the authors wrote.
In routine practice with the wide-area scanner, nodule PFMS represents the single most effective marker for distinguishing benign from malignant nodules -- including those with low and high expected biologic activity.
This information "could help physicians provide immediate treatment for patients with malignant nodules and help avoid surgery or further intervention for patients without malignant nodules," they wrote.
Limitations of the study include a large percentage (57%) of malignant nodules 30 mm or smaller, and a relatively large mean lesion size (15.9 mm ± 7.7). Patients were selected according to nodule criteria, introducing selection bias. The radiation dose needs to be reduced further and new tools are needed to accomplish this, they added.
"One might wonder whether, with use of the described recently developed area-detector CT system, the patients received unnecessary radiation on the basis of the size and the number of multiple nodules and the distance between the main trunk of the pulmonary artery and the nodules," the authors wrote. "This is because the detector collimation of current area-detector CT systems is not changeable for dynamic first-pass perfusion CT examinations and each scan always encompasses a 16-cm z-axis area."
The detector collimation for dynamic area-detector CT should be changeable according to the size and number of nodules and the distance between the main trunk of the pulmonary artery and the nodules to reduce the dose.
"In conclusion, dynamic first-pass area-detector perfusion CT might be more specific and accurate than integrated FDG-PET/CT in the differentiation of malignant and benign pulmonary nodules," Ohno and colleagues wrote. "Dynamic area-detector CT also might complement integrated FDG-PET/CT in the management of pulmonary nodules."
By Eric Barnes
AuntMinnie.com staff writer
February 16, 2011