In the quest for the sub-mSv CT exam, a number of methods can be called upon to reduce CT dose, presenters said in a summit sponsored by the U.S. National Institutes of Health (NIH), the American College of Radiology, and the Coalition for Imaging and Bioengineering Research.
In presentations at the two-day "NIH Summit to Focus on Management of Radiation Dose in Computerized Tomography" that wrapped up Friday in Bethesda, MD, radiologists shared how careful protocol design and implementation, organ dose estimates, dose simulation, and decision-support tools can help minimize the potential risks of ionizing radiation.
Among the speakers, Leslie Quint, MD, professor of radiology and surgery at the University of Michigan, said that careful CT protocol design and implementation can go a long way toward minimizing dose using currently available equipment.
Reducing unnecessary radiation means tailoring the CT exam to the specific clinical question and the specific patient being scanned, she said. There are four principal ways of achieving this goal:
- Confining scan volume to the region of interest
- Eliminating unnecessary scan series
- Scanning less frequently or substituting MRI or ultrasound when feasible
- Selectively using dose-reduction protocols
Confining the scan length to the proper upper and lower boundaries for the body part being scanned can cut the radiation dose by at least 20%, she said. Multiple studies show that more than 90% of exams acquire more anatomy than is required, and the literature suggests that the additional radiation "almost never results in clinically important information," she said.
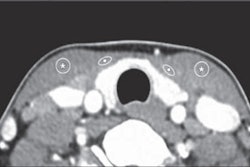
Soft tissues and vascular boundaries are the most frequent sites of superfluous scan coverage because they're harder to see on the scout image; more visible osseous boundaries are easier to follow. There are many sources of superfluous scanning, Quint said -- technologists sometimes acquire additional images, and radiologists often want to overdo to image the entire abnormality, none of which justifies unnecessary imaging.
"There is the potential for considerable radiation reduction by reducing extraneous imaging," she said. "There is a need to increase awareness among radiologists, ensure adequate tech training ... and consider very low-dose localizer scans for soft tissue or vascular boundaries."
Following up on lung nodules might properly be limited to a known nodule or cluster of nodules, she said, though it will require training and diligence to overcome the radiology mindset that generally concludes more scanning is better.
"It's more work for the radiologist," Quint said. "The techs won't be happy. It will slow throughput, but I think probably that it would be the right thing to do."
Similarly, stable aortic aneurysms could be followed up every two years rather than annually, as is done in her institution. CT urography can often be performed using a split bolus technique to acquire only an unenhanced and an excretory phase without the nephrographic phase, reducing the dose by 25%, she said.
MR enterography is often a good substitute for CT enterography, particularly in patients requiring frequent follow-up, she added.
Interstitial lung disease tends to be posteriobasilar, affecting only the lung apices to bases. So high-resolution CT (HRCT) follow-up can be limited to this region, she said.
Quint acknowledged barriers to a focus on minimizing the anatomic region covered in CT scans, in response to an audience member who cited a "cultural reluctance" of radiologists to do only single exams that focus on the body part being examined, as well as a desire to give patients their money's worth, and real or perceived medicolegal and reimbursement concerns.
More accurate organ doses
In his talk, Michael McNitt-Gray, MD, PhD, professor of radiology at the University of California, Los Angeles, talked about organ dose estimates and how to calculate them from the CT scanners' CT dose index readouts expressed in mGy. Organ dose estimates are a more accurate way to evaluate the real impact of radiation exposure on the patient, he said.
Organ doses could be tracked across scans and over time, and it's feasible to get estimates of cumulative organ dose over time. And now, for the first time, manufacturers are engaged in achieving easier and more automated organ dose reports, McNitt-Gray said.
Physicists tackle CT dose
Dianna Cody, PhD, chief of radiologic physics at MD Anderson Cancer Center and a member of the American Association of Physicists in Medicine's (AAPM) Working Group on Standardization of CT Nomenclature and Protocols, talked about that organization's work to develop optimized CT protocols.
AAPM has begun posting scan protocols for the most frequently performed CT exams on its website. The protocols -- though limited at this stage of the project -- summarize CT exam requirements and scanner-specific protocols, and provide examples of scanning and reconstructions that the working group considers reasonable to specific diagnostic tasks.
Before a new exam is posted, "we all look over the parameters and really carefully try and be sure they all make sense," Cody said. Due to the cost of providing such information, full access to the website is restricted to AAPM members.
Dose simulation tool
In his talk, Stanford professor of radiology Norbert Pelc, MD, discussed his group's vision for Synthetic CT Vision, a clinical tool "that would let radiologists and practitioners see what images would look like using a library of acquired data," he said. "These tools would let you change kVp, mAs, bow-tie filters, and even insert virtual objects to see what that would do."
Key to its functionality are dual-source CT scanners that create two separate sinograms for each image, Pelc said. The two raw datasets are then decomposed into basis materials.
Twisting the various control knobs, the radiologist can envision what a particular protocol would deliver before scanning, test new reconstruction algorithms, and provide a powerful educational tool. Implementation will require a massive database of samples, however, along with further validation of the techniques in different imaging environments, Pelc said.
Decision support
Decision-support algorithms will be an important contributor to reducing unnecessary scanning, said Steven Seltzer, MD, chair of radiology at Brigham and Women's Hospital in Boston. Even the systems available today are able to confirm the medical necessity of scans and eliminate duplication and waste, he said.
With greater implementation of the electronic health record (EHR) in the coming years, these systems will be increasingly useful in tracking cumulative radiation doses, Seltzer said. During the test they will ensure proper protocol selection and optimal equipment selection, calculating the patient's radiation exposure and uploading it to the EHR.
Brigham and Women's now uses decision support in more than 98% of its imaging orders, according to Seltzer. The system questions about 5% of scan requests, after which 4.9% are eventually dropped. Decision-support tools will also increasingly help with reimbursement in an age where preauthorization is ubiquitous.
Implementation of more advanced systems will require substantial investment in databases and the infrastructure to support their delivery, he said. They can help the radiologist choose the best imaging protocols.
Promise and drawbacks
In a panel discussion following the February 24 afternoon sessions, participants talked about the promise and drawbacks of the dose-reduction techniques.
The databases for decision-support models are expensive, and implementation lags several years behind discovery of the information, said one participant.
Don't institute reference doses, said another. To work on all scanner models, they will need to be unreasonably high and paradoxically could serve to increase the dose in many situations, he said.
Tracking exposures over time means exposing radiology to the possibility of using the information incorrectly, another participant added.
Reducing the dose in a variety of clinical settings means having ready access to hundreds of scan protocols. New CT scanners should come preloaded with software to help radiologists choose optimal scan settings for each imaging scenario.