The key imaging components of cystic fibrosis of the lungs are bronchiectasis and air trapping. For evaluating both, CT remains far and away the superior imaging modality despite radiation concerns, and despite recent improvements in MRI techniques, according to a study from Italy and the Netherlands.
Chest CT -- commonly acquired using low-dose end-inspiratory and end-expiratory images -- is the gold standard for CT follow-up in cases of cystic fibrosis (CF). The protocol provides approximately 1 mSv of radiation, or about a third of the U.S. background radiation for a year.
"However, the cystic fibrosis population consists of children and young adults who are the most sensitive to radiation," said Dr. Perluigi Ciet from Foncello Hospital in Italy. For these reasons, MRI has been suggested as an alternative method for cystic fibrosis follow-up, but literature on the modality's value in this application is equivocal.
The research team from Italy and the Netherlands decided to do a head-to-head comparison between MRI and CT for cystic fibrosis to monitor both air trapping (AT) and bronchiectasis (BE) at follow-up. They presented their results at the 2011 European Congress of Radiology (ECR).
The researchers examined 40 stable cystic fibrosis patients (20 female; mean age, 16.7 years) who all underwent chest CT and MRI studies. Patients received CT and MRI scans on the same day.
The MRI protocol (Avanto, Siemens Healthcare) consisted of a syngo Blade proton-density transversal (TR/TE/alpha: ∞/28 msec/180°) sequence. Low-dose 64-detector-row CT (Somatom, Siemens) consisted of volumetric end-inspiration and end-expiration images.
To compare the two modalities, the CT and MR images were anonymized and scored in random order by two independent observers using the CF-CT score and an equivalent CF-MRI score. Scores were expressed as a percentage of the maximal score. Statistics included Pearson, intraclass coefficient (ICC), Bland-Altman plots, and results mean (range).
"On the ICC plot, agreement was pretty good for CT but lower for MRI, so it was more difficult to score the MRI for the radiologists," Ciet said.
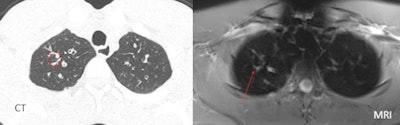 |
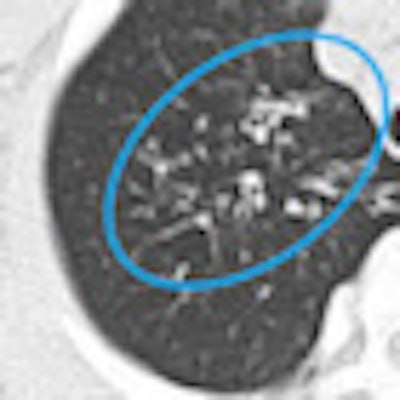
| Sometimes MRI was misleading, as in the case of a 22-year-old male patient with mild cystic fibrosis disease. Vessel depiction in MRI mimicked a large bronchiectasis of the right upper lobe. Moreover, MRI propeller sequence produced linear artifacts that derive from k-space reconstructions. The artifacts appear as lines in the lung parenchyma, creating false bronchi. All images courtesy of Dr. Perluigi Ciet. |
ICC showed greater interobserver variability for MRI in measuring bronchiectasis (CT-BE was 0.931, compared with 0.892 for MRI-BE). Air trapping showed even greater differences on the ICC plot, with CT-AT of 0.917 versus MRI-AT of 0.677.
Similarly, the Bland-Altman plots showed that for mild cystic fibrosis lung alterations, MRI overestimated bronchiectasis and air trapping compared to CT. And for severe cystic fibrosis lung alterations, MRI underestimated bronchiectasis and air trapping compared to CT.
"This means that with mild disease, MRI tends to overestimate [severity] compared to CT, and for severe disease, MRI tends to underestimate compared to CT," Ciet said. "And this was true for all of the components of air trapping."
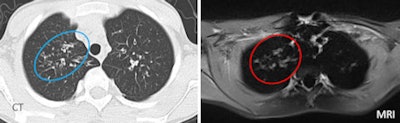 |
| MRI often overestimated mild disease, as in the case of a 24-year-old male patient with mild cystic fibrosis. In this patient, some small bronchiectasis of the right upper lobe (CT, left) appeared as a large area of mucus plugging (at MRI, right), resulting in an overestimation of the mucus score. This occurred because the wall thickening was blurred in the MR image, mimicking mucus plugs. |
The main limitation for MRI is in the lung periphery, Ciet said. It's already been shown (Falio et al, 2009) that MRI's spatial resolution degrades from the center of the lungs toward the periphery.
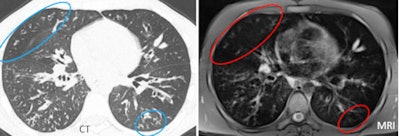 |
| MRI tended to underestimate the severity of disease at the lung periphery. |
"We found the same problem" as the earlier study, Ciet told AuntMinnie.com. "We saw disappearing anatomical structures like bronchiectasis, bullae [thin wall], and small plugs of mucus. Moreover it's quite difficult to differentiate between small mucus plugs and vessels at the periphery of the lung."
Only contrast media can be used to distinguish these two entities, as shown in previous research by Puderbach et al, he said, and no contrast was used in the present study. Ciet and colleagues also found evidence of MRI's lower spatial resolution versus CT.
"In MRI, it's easier to see all the anatomical changes that provoke an increase of the lung's density -- consolidation, large bronchiectasis with thick wall, large mucus plugs, etc. -- than those that determine a reduction of the lung density like air trapping," he said.
And MRI was unreliable for air trapping assessment, as shown in this study and previously by Heidelberg et al, he said.
Air trapping is an important sign of small airway disease, representing the main alteration in mild cystic fibrosis lung disease. The group is using an investigational sequence based on a Fourier decomposition technique supplied by the scanner manufacturer to work on this problem, Ciet said.
The group is also continuing to work with diffusion-weighted MRI as a tool to detect lung inflammation.
"I think that MRI has a large potential for functional lung imaging, and it's actually the main advantage versus CT," he said. Of course, functional imaging is also possible in CT and can be used to create ventilation maps.
"Despite the improvement, MRI still has lower spatial resolution than CT. MRI proved to be more problematic than CT," Ciet concluded. "At the same time MRI has a lot of potential to supply information by ventilation and perfusion, and other information that is really important in CF care."




















