
Men and women show important differences in the fat distribution patterns associated with metabolic syndrome as visualized on CT, according to a new study. The research was based on low-dose images acquired for virtual colonoscopy screening, hinting at potentially added value for VC studies.
Visceral fat was the most important predictor of disease in women, but subcutaneous fat was more important in men, according to the University of Wisconsin researchers. The group used low-dose CT images originally acquired for virtual colonoscopy screening in a population of nearly 500 adults, producing perhaps the most accurate diagnosis yet of the complex and troublesome condition.
Metabolic syndrome clusters several important risk factors for cardiovascular disease, including abdominal obesity, type 2 diabetes, hypertension, and dyslipidemia. However, current diagnostic methods are, in theory at least, very imprecise.
"If you look at the current diagnostic criteria for metabolic syndrome, one of key features is central obesity. But they measure it using waist circumference and [body mass index (BMI)], so the diagnosis doesn't differentiate where the fat is -- inside or outside," said Dr. Perry Pickhardt, associate professor of radiology at the University of Wisconsin, in an interview with AuntMinnie.com. Pickhardt presented the results last month at the European Society of Gastrointestinal and Abdominal Radiology (ESGAR) meeting in Venice, Italy.
The clinical criteria for diagnosis, established by the International Diabetes Federation (IDF), combine the central obesity measurement with two or more of the following: reduced HDL cholesterol, elevated triglycerides, elevated blood pressure, or elevated fasting plasma glucose. These factors make for "bad actors when they're clustered together," Pickhardt said.
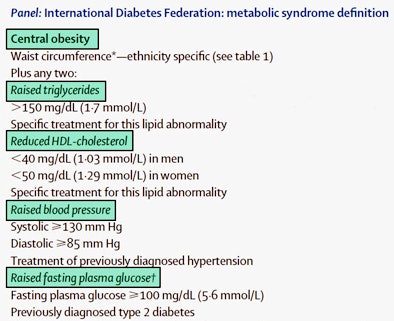 |
| International Diabetes Federation clinical criteria for the diagnosis of metabolic syndrome. All images courtesy of Dr. Perry Pickhardt. |
Metabolic syndrome is associated with an increased risk of cardiovascular events, and it has become an important health issue as its prevalence increases worldwide.
Two measures that are not part of the diagnostic criteria for metabolic syndrome are visceral adiposity and hepatic steatosis. However, research has singled them out for their key roles -- and, fortunately, CT is ideal for measuring them precisely, Pickhardt said.
"The subcutaneous fat compartment, visceral fat compartment, and liver are all well demonstrated at abdominal CT," he said.
The distribution of visceral and subcutaneous fat can be efficiently quantified at CT using a dedicated software tool, and measuring liver attenuation at noncontrast CT allows for noninvasive assessment of fatty liver disease. Nonalcoholic fatty liver disease has been strongly associated with the distribution of abdominal fat; however, waist circumference and BMI do not consider it.
The study sought to investigate the utility of abdominal fat and liver assessment at noncontrast CT in screening for metabolic syndrome. After excluding 127 patients for lack of data, the final study cohort included 474 (257 women, 217 men; mean age, 58.3 years), all asymptomatic adults who underwent VC (also known as CT colonography or CTC) screening over a 10-month interval.
The scans were acquired using low-dose noncontrast CT on a 16- or 64-detector-row CT scanner (LightSpeed series, GE Healthcare). The technique included 1.25-mm collimation, 120 kVp, and 50-100 mAs. The supine image series used to search for extracolonic findings was utilized for the study with 5-mm reconstructions, according to an abstract accompanying the presentation.
A previous study showed that colonic distention related to virtual colonoscopy doesn't meaningfully change the abdominal fat distribution categorization relative to routine CT. That means the results from CTC screening data are likely to be generalizable to more generic abdominal CT protocols used for the same secondary purpose, Pickhardt said. The present study used virtual colonoscopy images to assess the fat distribution, but any abdominal CT scan will do, he said.
In the search for steatosis or fatty liver, the group measured liver attenuation in HU using a validated method with a standard region of interest in the right hepatic lobe. Splenic attenuation was also recorded as a control dataset using the same method.
The researchers obtained semiautomated measurements of subcutaneous fat area (SFA), visceral fat area (VFA), and visceral fat percentage (VF% = 100 x VFA/[VFA+TFA]) at the umbilical level at noncontrast MDCT using a proprietary fat assessment tool (Philips Healthcare).
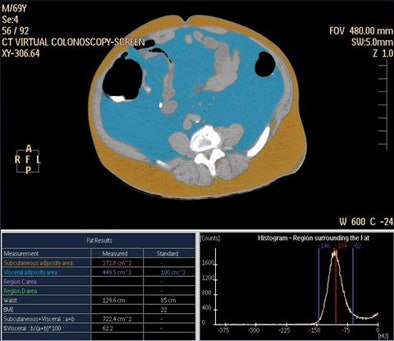 |
| Histogram-based fat assessment software distinguishes abdominal visceral fat (blue) from subcutaneous fat (brown). |
Logistic regression modeling was used to analyze the receiver operator characteristics (ROC) curve for predictors of metabolic syndrome. The researchers used Wilcoxon rank sum tests and Fisher's exact tests to evaluate differences between groups. Multivariate logistic regression modeling helped determine the optimal combination of predictors for metabolic syndrome.
The results showed that 168 of 474 participants met the IDF criteria for metabolic syndrome, an overall disease prevalence of 35.4%. The prevalence was similar between men and women.
For both men and women, visceral fat area was a strong predictor of metabolic syndrome, with area under the curve (AUC) values for VFA of 0.830 (95% confidence interval [CI]: 0.784-0.867) and 0.887 (95% CI: 0.848-0.918), respectively. The difference in AUC values between men and women was not statistically significant (p = 0.162).
In women, subcutaneous fat area was less predictive of metabolic syndrome, with an AUC of 0.762 (95% CI: 0.711-0.806). Subcutaneous fat area was a better predictor than visceral fat area for metabolic syndrome in men, with an AUC for SFA of 0.865 (95% CI: 0.823-0.899). The gender difference in AUC for subcutaneous fat area was significant (p = 0.0238).
"We found that men and women are very different," Pickhardt said. "I had kind of assumed the amount of visceral fat would be the best predictor of who is at risk of cardiovascular events, and sure enough, for women, visceral fat accumulation was an important predictor for things like diabetes and hypertension. But in men it was the amount of subcutaneous fat that was the best predictor."
In women, using a visceral fat area threshold of 70 cm2 yielded a sensitivity, specificity, and accuracy of 83.7%, 80.0%, and 81.3%, respectively. VFA performance was somewhat lower in men using a 125 cm2 threshold.
Among men, using the subcutaneous fat area at 204 cm2 yielded a sensitivity, specificity, and accuracy of 80.2%, 83.7%, and 82.4%, respectively.
Among women, an SFA threshold of 185 cm2 was sensitive (85.9%) but not specific (49.7%) for metabolic syndrome.
Unexpectedly, the visceral fat percentage was "like a coin flip," Pickhardt said -- with no statistical significance and, hence, no predictive power. Among men, the mean VF% for adults with and without metabolic syndrome were 37.1% and 35.7%, respectively (p = 0.516). In comparison, the mean VF% difference among women with and without metabolic syndrome was statistically significant (p < 0.001). VF% was a very poor predictor of metabolic syndrome among men, with an AUC of only 0.527 (95% CI: 0.472-0.581).
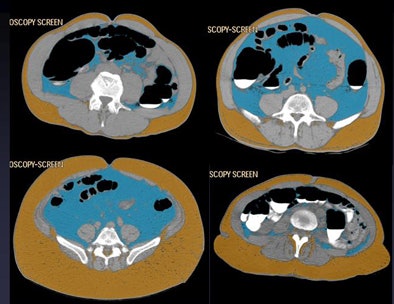 |
| Four patients show different abdominal fat distribution patterns. |
It is the first study the authors are aware of that found gender differences for fat distribution in metabolic syndrome, a finding that was made possible by using CT, Pickhardt said.
The large differences between the cohorts held true for most of the fat-based differences, particularly VFA in women, where the mean value for women with and without metabolic syndrome was 125 cm2 and 49.4 cm2, respectively (p < 0.001).
Fatty liver
"A lot of luminaries have suggested that for future directions with metabolic syndrome we need to look at the relationship of metabolic syndrome to fatty liver and fat distribution," Pickhardt said.
Still, the predictive value of the study was limited in that regard. The results showed that liver attenuation less than 50 HU was insensitive for metabolic syndrome (22.0%) but highly specific (96.7%), with a positive predictive value of 78.7% (37/47).
Even though sensitivity was low, if fatty liver is diagnosed, "your chances of having metabolic syndrome are quite high -- there were very few false-positives in that group," Pickhardt said, adding that the high positive predictive value is important in a screening test.
The combined area under the ROC curve for noncontrast liver attenuation was 0.706 (95% CI: 0.653-0.754) with similar performance among men (0.711) and women (0.706). Multivariate logistic regression modeling showed an AUC of 0.901 (95% CI: 0.864-0.930) but did not substantially improve performance over the best individual gender-specific individual measures.
Along with the gender-specific differences in the diagnosis of metabolic syndrome, fat distribution does seem to have an important predictive value for cardiovascular events, Pickhardt said.
Among the 429 participants (90.5%) who had complete cardiovascular event information, 50 (11.7%) had a documented cardiovascular event or complication. Of these 30 (60%) met the IDF criteria for metabolic syndrome and 20 (40%) did not. The association of metabolic syndrome and cardiovascular events, 19.6% (30/153) with metabolic syndrome versus 7.2% (20/276) without, was statistically significant (p < 0.001).
"People who had a lot of visceral fat -- even people who didn't qualify for metabolic syndrome but just had a lot of visceral fat -- had some of these complications, so it looks like it has some prognostic value," Pickhardt said.
Of the 20 patients with cardiovascular events who did not have the metabolic syndrome by IDF criteria, 11 (55%) had an elevated VFA using the gender-specific thresholds derived in this work. All but one of the 20 patients with events had BMI of 30 kg/m2 or less.
More research is needed to determine whether using fat distribution visualized at CT will lead to better diagnosis of metabolic syndrome and better predictions of risk, Pickhardt said.
This series doesn't answer all of the important questions unequivocally, but it's a "good first start to look at this," he said. "It's a fairly large series, and it's another tool radiologists can use to add value to virtual colonoscopy and to abdominal CT in general," as previous studies have done with VC and osteoporosis screening. "That's maybe the bottom line," he said.




















